-
PDF
- Split View
-
Views
-
Cite
Cite
Saad Alobaysi, Saud Alsairi, Abdullah Aljasser, Ahmad Alkhaddam, Abdullah Alshamrani, Iatrogenic injury to a vesicourachal diverticulum during laparoscopic appendectomy successfully managed conservatively, Journal of Surgical Case Reports, Volume 2019, Issue 10, October 2019, rjz293, https://doi.org/10.1093/jscr/rjz293
Close - Share Icon Share
Abstract
A vesicourachal diverticulum is a rare congenital anomaly that arises from the incomplete closure of the urachus at the bladder end. We describe a 12-year-old boy who presented with severe persistent right iliac fossa pain associated with subjective fever, nausea, vomiting, and anorexia. A computed tomography (CT) scan of the abdomen and pelvis revealed findings consistent with appendicitis. The patient underwent a laparoscopic appendectomy; however, his postoperative course was remarkable for a low urine output and urine leakage from the suprapubic port site. A CT cystography showed a vesicourachal diverticulum and conservative management was offered. This management consisted of Foley catheter placement, hourly monitoring of the patient’s urine output, antibiotic prophylaxis, daily laboratory investigations and a cystography performed after 7 days. Overall, injury to the vesicourachal diverticulum is rare, and surgeons should be aware of this rare clinical entity and exercise caution during port placement. Surgeons should also have a high index of suspicion to identify these injuries and appropriately manage the condition early.
INTRODUCTION
The urachus, also referred to as the median umbilical ligament, is a vestigial remnant lying between the transversalis fascia and the peritoneum. It results from the involution of the cloaca and the allantois, forming a fibrous cord that extends upward from the apex of the bladder and attaches to the umbilicus [1]. If the obliteration of the urachus is incomplete, disorders of the urachus can arise; however, urachal anomalies are rare and usually occur in children.
Urachal anomalies are categorized into following four groups: patent urachus, urachal cyst, umbilical urachal sinus and vesicourachal diverticulum [2]. Anomalies of the urachus are clinically silent and may be discovered fortuitously during a radiographic investigation for an unrelated reason or after a complication, such as a urinary tract infection or intraurachal stone formation. Injury to the vesicourachal diverticulum due to laparoscopic port placement is an extremely rare complication [3]. We report a case of iatrogenic injury of the vesicourachal diverticulum that was successfully managed conservatively.
CASE PRESENTATION
A 12-year-old boy old presented to the emergency department complaining of severe persistent right iliac fossa pain associated with subjective fever, nausea, vomiting and anorexia. On examination, his vital signs were found to be within normal limits. An examination of the abdomen revealed right iliac fossa tenderness and rebound tenderness.
Laboratory investigations showed following results: white blood cell count 24.00 × 103/μl (reference range 4.5–11), hemoglobin 13.6 g/dl (reference range 13–16), C-reactive protein 76.5 (<5 nl). A computed tomography (CT) scan of the abdomen and pelvis using oral and intravenous contrast showed a distended appendix filled with fluids (Fig. 1). Also observed were pockets of air with a larger proximal and smaller distal fecolith with free fluid in Morison’s pouch, right paracolic gutter and rectovesical pouch consistent with acute complicated appendicitis.
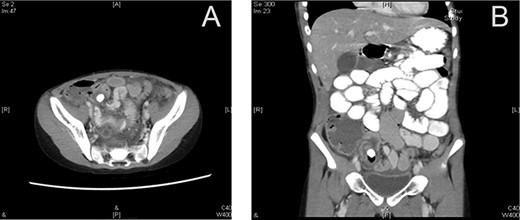
Preoperative CT scan (axial section) showing a dilated appendix with an enhanced wall filled with fluids and air pockets (A). A large appendicolith was noted. The coronal section shows a dilated appendix with an enhanced wall filled with fluids and air pockets. A large appendicolith was noted (B).
The patient underwent a laparoscopic appendectomy. Following three trocars were inserted: a 5 mm supraumbilical trocar, a 5 mm suprapubic trocar with a balloon and a 10 mm in the right lumbar area. The procedure was uneventful with no intraoperative complications. A 15 F drain was inserted through the suprapubic incision, and the patient was admitted to the surgical ward for observation.
The patient’s postoperative course was remarkable for a low urine output, which was noted on the night of his surgery. His supraoptic dressing was soaked with a clear yellow fluid, and the patient was complaining of mild suprapubic pain. An examination revealed suprapubic tenderness, and the drain contained 80 ml of a clear yellow fluid. The patient’s dressing was changed and closed, and his urine output was observed. The drained fluid was sent for analysis.
On a postoperative day 1, the suprapubic dressing was soaked with urine and the drain contained 200 ml of a clear yellow fluid. The patient did not urinate at all postoperative.
An abdominal examination revealed generalized guarding. A Foley catheter was inserted, and it yielded 275 ml of clear urine. A potential diagnosis was made for iatrogenic bladder injury.
A CT cystography was performed, and it showed a vesicourachal diverticulum. The suprapubic drain that was placed intraoperatively was shown to be penetrating the diverticulum (Fig. 2). The urology department was consulted and the patient’s condition was discussed with his family. Management options were offered, including conservative management with Foley catheter placement and operative repair; the family opted for conservative management. The management included hourly monitoring of his urine output, antibiotic prophylaxis with intravenous cefuroxime 625 mg thrice a day and intravenous metronidazole 350 mg thrice a day, daily laboratory investigations (complete blood count, renal function tests and serum electrolytes), and a cystography performed after 7 days. The patient’s daily urine output is shown in Table1.
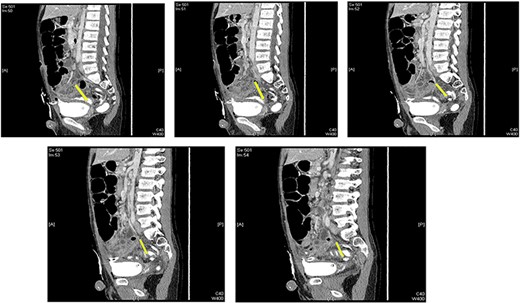
Multiple sagittal views showing the drain penetrating the urachus.
| Postoperative day . | Urine output (ml) . |
|---|---|
| 1 | 200 |
| 2 | 665 |
| 3 | 850 |
| 4 | 2280 |
| 5 | 1950 |
| 6 | 1540 |
| 7 | 950 |
| 8 | 850 |
| Postoperative day . | Urine output (ml) . |
|---|---|
| 1 | 200 |
| 2 | 665 |
| 3 | 850 |
| 4 | 2280 |
| 5 | 1950 |
| 6 | 1540 |
| 7 | 950 |
| 8 | 850 |
| Postoperative day . | Urine output (ml) . |
|---|---|
| 1 | 200 |
| 2 | 665 |
| 3 | 850 |
| 4 | 2280 |
| 5 | 1950 |
| 6 | 1540 |
| 7 | 950 |
| 8 | 850 |
| Postoperative day . | Urine output (ml) . |
|---|---|
| 1 | 200 |
| 2 | 665 |
| 3 | 850 |
| 4 | 2280 |
| 5 | 1950 |
| 6 | 1540 |
| 7 | 950 |
| 8 | 850 |
A contrast cystogram was performed on postoperative day 9, and a pelvic scan showed no leak or extravasation of the contrast fluid (Fig. 3). The catheter was removed, and the patient was discharged after successful micturition trials. Follow-up examinations performed 2 weeks and 1 month post-discharge were unremarkable and the patient presented no complaints.

Cystogram performed on postoperative day 8 showed no extravasation of the contrast material.
DISCUSSION
A vesicourachal diverticulum is a congenital urachal anomaly that arises from the incomplete closure of the urachus at the bladder end. It is reported to constitute about 3–5% of all urachal anomalies and manifests as an outpouching from the anterior dome of the bladder at the point where the urachus attaches the apex to the anterior abdominal wall [2]. Vesicourachal diverticula are typically large and drain well into the bladder. Consequently, most of the patients remain asymptomatic and the anomaly is only discovered fortuitously during a radiographic examination performed for other reasons [2]. In our patient’s case, the anomaly was discovered only after a CT cystography performed for postoperative urine leakage showed injury to the vesicourachal diverticulum caused by the placement of a suprapubic drain.
Iatrogenic injury to the vesicourachal diverticulum is an extremely rare finding, with less than 10 cases reported during the last decade [3–5]. The most recent case was reported in 2015 in a 10-year-old boy who underwent a laparoscopic appendectomy for appendicitis [3]. Similar to our case, the injury was not recognized during surgery and was only identified after a CT cystogram was performed for suspicion of a bladder injury. A high index of suspicion by the surgeon remains the key to diagnosing bladder injury [6]. During surgery, the injury can be recognized by the leaking of urine at the port insertion site or by the presence of blood or air in the urinary catheter [7]. However, if the surgeon fails to recognize the injury intraoperatively, the diagnosis might be uncertain postoperatively because patients typically present nonspecific symptoms due to the resulting urinary peritonitis and may have signs suggestive of acute kidney failure [8].
The morbidity of unrecognized bladder injury is high [4]. Unfortunately, clinicians have a low index of suspicion in cases of urachal injury because they have limited experience with these types of injuries. Consequently, the diagnosis is usually made several days later [8]. Patients may complain of abdominal or low back pain and may show signs of peritoneal irritation or peritonitis 1–4 days after injury [8]. The patient in our case complained of mild suprapubic pain 1 day after surgery, and an examination of the abdomen revealed suprapubic tenderness. The diagnosis was only reached after a CT cystography showed that the suprapubic drain placed intraoperatively was penetrating the diverticulum. Ultrasound, CT, and magnetic resonance imaging can all identify a vesicourachal diverticulum as a midline focal protruding extension of the bladder that arises from its dome and does not communicate with the umbilicus or the urachal tract [2]. A voiding cystourethrography can also demonstrate a tubular structure filled with contrast material extending from the superior part of the anterior bladder dome.
The management of bladder injuries depends on various factors, including the size of the injury, its location and the diagnostic approach. Cases that are recognized intraoperatively should be repaired during the procedure. However, several techniques have been recommended for injuries that are diagnosed postoperatively. Conservative management, through urinary catheterization, can be offered to patients with grade 2 urinary injuries, whereas surgery is recommended for those with grades 3 to 5 injuries [9]. There are no specific treatment recommendations for cases that are discovered fortuitously. The clinician should consider the potential of malignancy for remnants with epithelium [10]. Several management strategies have been reported for patients with iatrogenic injury to a vesicourachal diverticulum, ranging from prolonged catheterization of the bladder [4] to surgical repair [8] to resection of the diverticulum followed by suturing of the bladder defect [3]. Our case was successively managed conservatively. A Foley catheter was placed within a few hours after diagnosis, and other elements of management included hourly monitoring of the patient’s urine output, antibiotic prophylaxis, daily laboratory investigations, and a cystography performed after 7 days.
In conclusion, a vesicourachal diverticulum is the least frequent type of urachal anomaly. However, cases of vesicourachal diverticulum may be underreported because patients are usually asymptomatic. The diagnosis is typically made fortuitously during imaging. Although the intraoperative diagnosis is key to diagnosing the condition, many physicians may miss it, thereby delaying diagnosis. Nevertheless, the condition can be successfully managed with prolonged indwelling catheterization or surgical repair.
REFERENCES
- anorexia nervosa
- antibiotic prophylaxis
- congenital abnormality
- appendicitis
- computed tomography
- exercise
- fever
- diverticulum
- ilium
- oliguria
- pain
- abdomen
- urinary bladder
- pelvis
- urachus
- urine
- urine volume
- persistence
- cystography
- foley catheters
- nausea and vomiting
- iatrogenic injuries
- appendectomy, laparoscopic
- loss of appetite
- conservative treatment



