-
PDF
- Split View
-
Views
-
Cite
Cite
Aghyad Kudra Danial, Muhamad Zakaria Brimo Alsaman, Rama Zazo, Muhammad Mazketly, Mohammad Nour Kitaz, Majd Alobied, Nihad Mahli, A unique case of congenital transmesocolic hernia with malrotation in a 25-year-old female: a case report, Journal of Surgical Case Reports, Volume 2019, Issue 10, October 2019, rjz280, https://doi.org/10.1093/jscr/rjz280
Close - Share Icon Share
Abstract
Congenital transmesocolic hernia of the transverse colon is a very rare type of internal hernia. In addition, intestinal malrotation is very rare in adults. Most of these patients do not have clear clinical manifestations. Incidence of congenital transmesocolic hernia of the transverse colon along with malrotation is an unusual phenomenon in medical literature and clinical practice. Here, we report a unique case of a 25-year-old woman diagnosed with transmesocolic hernia of the transverse colon and malrotation of the small intestine, without any history of trauma or previous surgery. The patient underwent surgery, where the hernia orifice was closed and Ladd’s procedure was performed.
INTRODUCTION
Internal hernia is a protrusion of visceral contents through an opening within the peritoneal cavity. It can be classified into many groups such as paraduodenal, pericecal, intersigmoid and transmesocolic (which is a very rare type of internal hernia) [1]. The reported incidence of internal hernias ranges from 0.2 to 0.9%, and they are responsible for about 0.5–5% of all intestinal obstruction [2]. Transmesocolic hernia accounts for approximately 5–10% of all internal hernias [1].
Transmesocolic hernia of the transverse colon is very rare and the majority of it could result from congenital anomalies or acquired defects secondary to abdominal surgery or trauma [1].
On the other hand, intestinal malrotation occurs when the normal rotation of the embryonic gut has not completed during embryonic development [3]. However, adult midgut malrotation is rare with an incidence ranging from 0.0001 to 0.19% in asymptomatic adults [4].
CASE PRESENTATION
A 25-year-old female with no previous medical or family history, abdominal surgery, injury or peritonitis presented to the clinic complaining of recurrent intermittent abdominal pain with dyschesia, nausea and constipation. The pain has started 2 years ago and did not respond to medication.
Physical examination revealed mild abdominal distension, mild tenderness in the periumbilical region, tympanites in the left side of the abdomen and no loss of weight. Abdominal ultrasonography showed a mild amount of serous fluid in the abdomen and pelvis, the abdominal X-ray (AXR) showed air-fluid levels within the transverse colon and absence of gases in the pelvis (Fig. 1), chest X-ray and laboratory tests were normal.

AXR shows air-fluid levels within the transverse colon and absence of gases in the pelvis.
The patient was kept under conservative treatment (intravenous fluids, anti-vomiting and nasogastric tube) and was diagnosed with subacute intestinal obstruction.
After 24 h of conservative treatment, the abdominal pain escalated with rebound tenderness in the umbilical region and no bowel movements.
Diagnostic laparoscopy with three trocars (10-mm trocar across the umbilicus, 5-mm trocar across the right hypochondrium and 5-mm across the left hypochondrium) was performed in the front abdominal entrance under general anesthetization, and the findings were serous fluid in the pelvic cavity (100 mL).
Laparoscopic surgery was excluded for technical and anatomical difficulties; we switched to open surgery. During intraoperative, we found malrotation (90° counterclockwise), where the small intestine was on the right side and the colons were on the left side (Fig. 2), and small intestine was slightly dilated and entrapped within a congenital hernia in the mesentery of the transverse colon (Fig. 3).
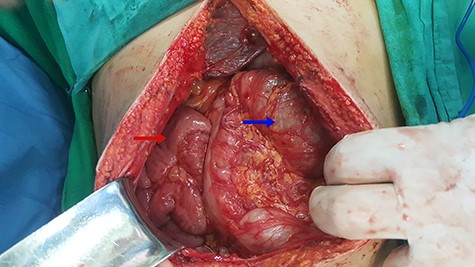
Red arrow indicates to the small intestine and blue arrow indicates to the colons.

Small intestinal entrapped within a congenital transmesocolic hernia.
We extracted the small intestine from the hernia orifice and reversed it to the normal anatomical position using Ladd’s procedure. After we repositioned colons and cecum, we closed the orifice of hernia. Finally, we fixed the right colon and performed an appendectomy.
On the first day after surgery, there were normal intestinal movements, positive abdominal gas and an absence of nausea and vomiting. The patient was kept under intravenous fluids, analgesics and H2 histamine receptor antagonists for the first day. After 2 days of following up, the patient was doing well, and her AXR was normal.
DISCUSSION
The internal hernia may occur if there is a congenital mesenteric defect or a part of the small intestine becomes entrapped in one of the retroperitoneal fossae [3]. Congenital internal hernia considered a rare cause of bowel obstruction [5]. Transmesenteric hernias are a rare type of congenital internal hernia, and it is divided into two types: transmesocolic and transomental, both of which are rare [1]. The most probable reasons for transmesocolic hernias are previous surgery, abdominal trauma or intraperitoneal inflammation [1].
We report a unique case of a 25-year-old female that was diagnosed with congenital transmesocolic hernia of the transverse colon and malrotation, without any history of trauma or previous surgery. Incidence of congenital transmesocolic hernia of the transverse colon along with malrotation is an unusual phenomenon in medical literature and clinical practice.
Clinical manifestations are not clear but the majority of patients present with symptoms of acute or intermittent small bowel obstruction, and therefore, the preoperative diagnosis of internal hernia is quite difficult [6]. In general, investigations for hernia are made by plain radiographs of the abdomen, ultrasound scan, ultrasonography, computed tomography and magnetic resonance imaging [3].
Although the diagnosis of transmesocolic hernia is difficult to establish, CT scan might help to confirm the diagnosis. It shows elongation, grouping and engorgement of the mesenteric vessels, displacement of the mesenteric trunk toward the hernia, abnormal encapsulation of intestinal loops in the peritoneal cavity, stasis, and absence of intraluminal contrast progression associated with distension content [5, 7]. Laparotomy and laparoscopy are performed to manage the internal hernia [6]. Congenital anomalies of intestinal rotation are very rare in adults with an incidence ranging from 0.0001 to 0.19% in asymptomatic adults; however, most cases are seen in infants, and it is found incidentally at laparotomy [4, 8].
Left-sided colon results from gut rotation defects during embryonic development where intestinal loop rotates only 90° instead of 270° counterclockwise, thereby positioning the small intestine on the right side and the large intestine on the left side. It occurs by the 12th week of gestation [3].
It is difficult to diagnose malrotation in adults because of its rare incidence and most adults remain asymptomatic throughout their lives. They may present with obstruction and ischemia associated with volvulus or chronic abdominal pain [4, 9].
Our patient was complaining of recurrent intermittent abdominal pain, dyschesia, nausea and constipation.
Also, investigations for malrotation are performed by plain radiographs of the abdomen, but they are not useful, and contrast-enhanced CT scan is considered to be the investigation of choice in adults [10].
In addition, an upper gastrointestinal contrast study affirms malrotation. Surgical management, which is called “Ladd procedure,” is performed to manage intestine malrotation at any age [3].
The patient underwent surgery, where the hernia orifice was closed and Ladd’s procedure was performed to reverse the small intestine to the normal anatomical position.
Conflicts of Interest Statement
None declared.
Ethical approval
Not required for case reports at our hospital. Single case reports are exempt from ethical approval in our institution.
Consent
Informed consent was obtained.



