-
PDF
- Split View
-
Views
-
Cite
Cite
Toyin A Oyemolade, Augustine A Adeolu, Olusola K Idowu, Spinal extradural arachnoid cyst in a child—a case report, Journal of Surgical Case Reports, Volume 2019, Issue 10, October 2019, rjz283, https://doi.org/10.1093/jscr/rjz283
Close - Share Icon Share
ABSTRACT
Extradural spinal arachnoid cysts are rare lesions. They frequently communicate with the subarachnoid space through a defect in the dura. Symptoms result from compression of the spinal cord or nerve roots. The treatment of choice is complete surgical excision. We report the case of a 12-year-old girl with extradural spinal arachnoid cyst who had complete surgical excision with good outcome.
INTRODUCTION
Spinal arachnoid cysts are uncommon, accounting for about 1% of all primary spinal mass lesions. They can be extradural or intradural in location. Extradural spinal arachnoid cysts are rare lesions with still unclear pathogenesis [1–3]. They are predominantly found in the thoracic spine, followed by the lumbosacral and thoracolumbar regions [4–6]. They are characterized by a wide range of clinical manifestations, from asymptomatic lesions to severe myelopathy [7]. It is difficult to state precisely the incidence since only few cases have been reported, and a significant proportion are asymptomatic, thus are detected accidentally on magnetic resonance imaging (MRI). Surgical intervention is indicated in symptomatic cases with a generally satisfactory outcome [1]. To the best of our knowledge, there has been no report of an extradural spinal arachnoid cyst from our country. We present a 12-year-old girl with spinal cord compression caused by a thoracic extradural spinal arachnoid cyst.
CASE REPORT
This 12-year-old girl presented with progressive lower limb weakness of eleven months duration, with associated spasms and paraesthesia. There was no back pain or sphincteric dysfunction. She was ambulating with crutches at presentation. Neurological examination revealed spastic paraparesis, with power grade 3–4 in most muscle groups of the lower extremities. Muscle stretch reflexes were brisk with un-sustained ankle clonus and extensor plantar response bilaterally. Thoracic spine MRI showed a cystic lesion compressing the spinal cord posteriorly from T4–T8 (Fig. 1). We performed a T4–T8 laminectomies and total excision of the cyst. The cyst communicated with the subarachnoid space through a pedicle located dorsolaterally at T7 close to the nerve sleeve (Fig. 2). The dura defect was repaired without duroplasty. There was no complication. She made remarkable post-operative improvement and was ambulating without support at the time of discharge. She was last seen at the outpatient clinic 18 months after surgery. The post-operative neurological improvement was sustained; the power was grade 5 in all muscle groups of the lower limbs (Fig. 3).
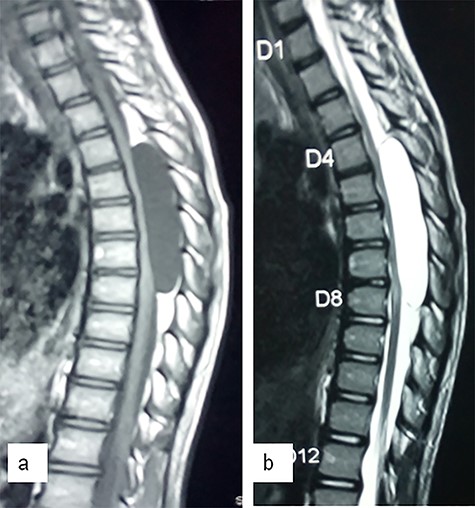
Sagittal T1 (a)- and T2 (b)-weighted MR images showing a large cystic lesion at T4–T8 compressing the spinal cord.
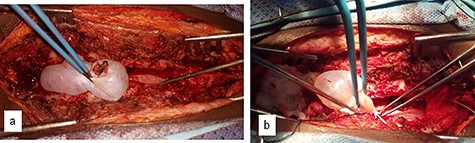
Intraoperative images showing dissection of the cyst from the dura (a) and the point of communication with the subarachnoid space (arrow) (b).

DISCUSSION
Spinal meningeal cysts have been classified by Nabors et al. into spinal extradural meningeal cyst without nerve root fibres (type I), spinal extradural meningeal cyst with nerve root fibres (type II), and spinal intradural meningeal cyst (type III). The type I cysts are subdivided into type IA (spinal extradural arachnoid cyst) and type IB (occult sacral meningocele). The type II cyst is also known as Tarlov perineural cyst or spinal nerve root diverticulum, while type III cyst is spinal intradural arachnoid cyst. Extradural spinal arachnoid cysts are rare lesions. The aetiology and pathogenesis of these lesions are yet to be fully defined in the literature [1, 3, 7, 8]. The pathogenesis is, however, different from intradural cysts [4]. The proposed origin include congenital defect in the dura; however, association with arachnoiditis, trauma and surgery has been reported [1, 2, 8, 9]. In our case, there was no history of trauma or spine surgery, therefore most likely of congenital origin. These lesions are predominantly located in the thoracic region accounting for about 65% of the cases but have also been found in the lumbar and lumbosacral (13%), thoracolumbar (12%), sacral (7%) and cervical regions (3%) [1, 3–7]. They are more commonly located dorsal to the spinal cord, but may also be ventrally located [10]. The cysts communicate with spinal subarachnoid space through a pedicle, the location of which varies from dorsal midline to root sleeve [2, 5]. In this case, the cyst was located dorsally in the middle thoracic region and communicated with the subarachnoid space through a pedicle located dorsolaterally close to the dura sleeve. Extradural arachnoid cysts may sometimes be asymptomatic [1, 7]. When symptomatic, however, symptoms result from compression of the spinal cord or nerve roots [1, 4]. The location and size of the cyst determines the severity of the symptoms [1, 2]. The duration of symptoms is shorter in the thoracic spine because of smaller diameter of the spinal canal at this level [10]. MRI is the imaging modality of choice as it can accurately localize the cyst and can show the size and degree of neural tissue compression [1, 2, 7]. On all sequences of MRI, arachnoid cysts’ signal intensity is the same as that of cerebrospinal fluid. Failure to clearly delineate the cyst walls suggests intradural arachnoid cyst. This imaging modality can also help to differentiate arachnoid cyst from other spinal cysts, abscess or cystic tumours. Epidermoid and dermoid cysts often have inhomogenous signal intensity with contrast enhancement of the walls. Synovial cysts are usually small and originate from facet articulation. Abscesses show restricted diffusion on diffusion-weighted MRI, while cystic tumours show contrast enhancing solid parts. Asymptomatic patients can be managed by clinical and imaging follow-up. Surgical intervention is indicated in symptomatic cases or when the cyst is located ventral to the cord, because of ischaemic risk of the compression in this region [1, 7]. Several surgical approaches have been proposed including: aspiration, fenestration of the cyst wall, placement of a shunt (cystopleural, cytoperitoneal or cystosubarachnoid) and resection of the cyst wall [1, 3, 4, 8]. The treatment of choice is complete excision of the cyst, obliteration of the communicating pedicle and watertight repair of the dural defect to prevent recurrence [4, 8]. When this is not feasible because dense fibrous adhesions prevent safe separation of the cyst from the dura, a wide marsupialization of the cyst can be performed by resecting the dorsal wall of the cyst and closing the dural defect. When dura defect is large, duroplasty is needed to close the defect [8]. Our patient had complete excision of the cyst with primary repair of the dura defect. Simple cyst aspiration has not been found to be effective. Likewise, failure has been reported with placement of shunt [4].
CONCLUSION
Spinal extradural arachnoid cysts are rare causes of spinal cord compression with only few reported cases in the literature. They are mostly located dorsally in the thoracic region and cause symptoms by spinal cord or nerve root compression. The operative technique of choice is complete excision of the cyst, obliteration of the communicating pedicle and watertight repair of the dural defect to prevent recurrence.
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interests.



