-
PDF
- Split View
-
Views
-
Cite
Cite
Rathin Gosavi, George Balalis, Andrew Packiyanathan, Mischievous gastric band port: a rare and delayed presentation, Journal of Surgical Case Reports, Volume 2019, Issue 10, October 2019, rjz278, https://doi.org/10.1093/jscr/rjz278
Close - Share Icon Share
Abstract
Bowel perforation is a rare and unusual complication of laparoscopic adjustable gastric band (LAGB) insertion, which if left undiagnosed can have potentially fatal consequences. We present the first case ever published of a delayed presentation of small-bowel perforation secondary to a laparoscopic port insertion. A young woman presented to Emergency Department with intermittent vague abdominal pain for 5 months, on the background of having a LAGB inserted 4 years prior. She was subsequently found to have a small-bowel perforation with mesenteric adhesions to a laparoscopic port site. The patient underwent a successful small-bowel resection with primary anastomosis and made an uneventful recovery.
INTRODUCTION
Obesity remains one of the greatest public health risks in the developed world. In Australia, the prevalence of obesity (body mass index > 30) has been steadily increasing with 1 in 10 more adults obese today compared to 1995 [1]. Bariatric surgery has been shown to be effective, especially in those who have not achieved sustainable weight loss from dietary, lifestyle and pharmacological interventions [2]. The laparoscopic adjustable gastric band (LAGB) gained popularity as it is a minimally invasive procedure with adjustability, reversibility and a quick post-operative recovery. It is, however, not without complications, some potentially life-threatening.
CASE REPORT
A 24 years old woman presented to ED with intermittent vague upper abdominal pain, nausea and malaise for 5 months. Her past history was only significant for obesity, for which she had an LAGB inserted over 4 years ago. Her blood tests on presentation revealed a white cell count of 8.46 109/L and a C-reactive protein of 28 mg/L with haemoglobin, platelets, electrolytes and liver enzymes all being within normal limits, as were her vitals. An abdominal examination revealed a focal tenderness over her periumbilical area and surrounding the well-healed LAGB port site. Computed tomography scan (Fig. 1a and b) showed an abnormal port position with soft tissue thickening seen surrounding the tube within the subcutaneous tissues of the abdominal wall and for a short distance within the abdomen and a segment of small bowel immediately deep to the entry. Findings were highly suspicious for a peritubal infection and/or a small-bowel perforation.
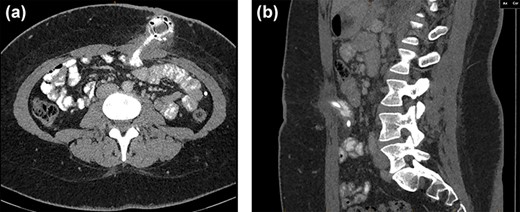
CT axial (a) and sagittal (b) views showing soft tissue thickening surrounding the LAGB port within the subcutaneous tissues of the abdominal wall extending to a segment of small bowel.
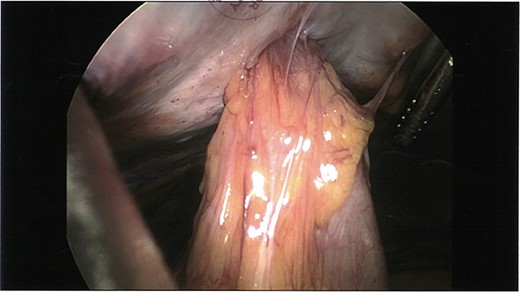
Initial laparoscopic view of the loop of small bowel tethered to the anterior abdominal wall.
The patient was taken to theatre for a diagnostic laparoscopy where a loop of small bowel was found tethered to the anterior abdominal wall (Fig. 2). A decision was made for a local transverse incision over collection and the sinus tract was excised to find a small-bowel perforation around the RapidPort with an abscess cavity extending through the subcutaneous tissue to the skin. The bowel was run and no other areas of compromise were noted. Additionally, there was no evidence of soft tissue injury and the omentum appeared intact. The patient underwent a successful small-bowel resection and made an uneventful recovery. Histopathology confirmed a full-thickness defect in the resected small bowel segment with adjacent acute serositis.
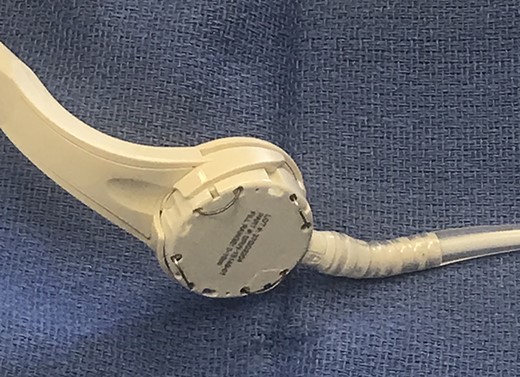
We deduce that during the primary LABG insertion procedure, a loop of small bowel and its accompanying mesentery was unknowingly caught in the expandable prongs of the laparoscopic RapidPort (Fig. 3) and hitched to the anterior abdominal wall. On the removal of this port, it appears that the segment of small bowel remained tethered with perforation contained within the abdominal wall.
DISCUSSION
Morbid obesity is a significant clinical issue in the western world. LAGB insertion is a popular surgical option for the management of obesity and related metabolic diseases as it is a minimally invasive, effective and safe technique with the added benefit of being reversible [3, 4]. The procedure, however, is not without complications and although rare can be associated with including band slippage, band erosion, oesophageal dilatation, pouch enlargement and prosthesis infection [5, 6].
Our case highlights the importance of delayed bowel injuries as they can present insidiously with non-specific symptoms and normal bloodwork. We advise surgeons to be more vigilant of both intraoperative port placement and clinical assessment post-operatively.
Conflict of Interest STATEMENT
None declared.
REFERENCES



