-
PDF
- Split View
-
Views
-
Cite
Cite
Catarina Moura, Luís Amaral, Joana Mendes, Rui Quintanilha, Francisco Melo Bento, Maria Inês Leite, António Melo, Hepatic rupture in HELLP syndrome, Journal of Surgical Case Reports, Volume 2019, Issue 10, October 2019, rjz277, https://doi.org/10.1093/jscr/rjz277
Close - Share Icon Share
Abstract
HELLP syndrome is a rare complication of pregnancy that may result in serious consequences such as hepatic rupture, one of the most feared and potentially life-threatening complications. This article aims to carry out a literature review on hepatic rupture in the context of HELLP syndrome as well as to present two clinical cases.
INTRODUCTION
Hepatic hematoma and rupture are rare complications of HELLP syndrome, first described by Weinstein in 1982. It is characterized by microangiopathic hemolysis, thrombocytopenia and impaired hepatic function [1]. It commonly occurs between 28 and 36 weeks of gestation, but it can also occur postpartum or even during labor [2]. It is associated with a maternal mortality rate of 3.3%. However, when hepatic hematomas are present, or when hepatic rupture develops, mortality and morbidity rise significantly [3].
From a clinical perspective, hepatic hematomas are characterized by pain in the right hypochondrium or epigastrium (70–90% of cases), though other symptoms may be associated [4]. Given their rarity and variable presentation, diagnosis delays are frequent, which may pose serious consequences [1].
Management mainly consists of eliminating the causal factor, pregnancy termination and controlling hemorrhage. In turn, this depends on the hemodynamic status and the severity of the hepatic lesion [5].
In case of a hemodynamically stable patient with hepatic hematoma, the hematoma does not require specific surgical treatment. In case of a hemodynamically unstable patient or with diagnosis of hepatic rupture, a median laparotomy should be performed [5].
Regarding surgical management, the approach should respect the same principles of trauma surgery. The course of action involves controlling the hemorrhage and, after hemostasis, proceeding with the definitive treatment in the same or subsequent surgery [6].
Several surgical options have already been described: electrocoagulation, hemostatic agents, hepatic artery ligation, hepatic packing, hepatic suture, anatomical or non-anatomical resection, prostheses and, in extremis, liver transplantation [3, 7, 8]. A less aggressive surgical approach is preferable compared to major surgical interventions [7].
CLINICAL CASE 1
Thirty-year-old pregnant woman, with a history of hypertension and obesity, was admitted at 38 weeks gestation in labor. Her pregnancy follow-up registered no intercurrences. The two previous pregnancies were without complications.
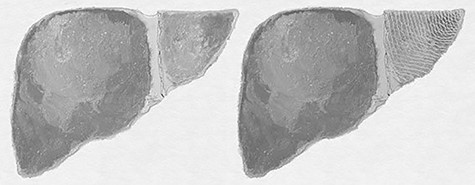
Clinical case 1 – Vicryl® prosthesis involving the left lobe (illustration).
During labor, the patient presented with sudden onset of pain in the right hypochondrium with irradiation to the homolateral shoulder. On admission, the patient was hemodynamically stable. Blood work revealed anemia (10 g/dl), thrombocytopenia (60 × 103/μl) and impaired hepatic function (AST 209 U/L, ALT 164 U/L, LDH 717 U/L).
An emergency c-section was performed, during which a massive hemoperitoneum was observed. It was subsequently converted to median laparotomy and a subcapsular hepatic hematoma involving the entire left lobe was found, with rupture and active hemorrhage. Hepatic packing was performed. However, the patient continued to bleed profusely. Therefore, a Vicryl® prosthesis involving the left lobe was placed to effectively control the hemorrhage (Fig. 1).
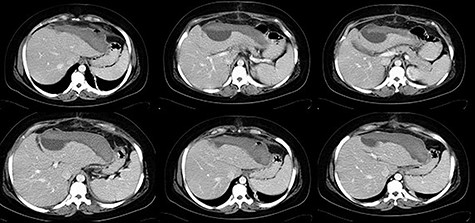
The postoperative period was favorable with lesion regression in serial Computed tomography scan control and was discharged on the 13th postoperative day (Fig. 2).
CLINICAL CASE 2
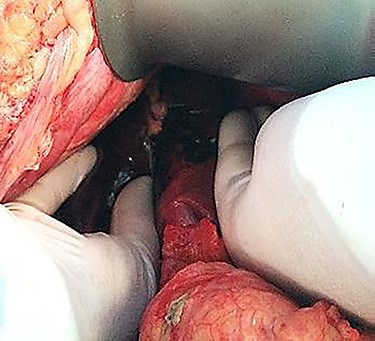
Thirty-one-year-old pregnant woman, primigravida, with history of obesity, admitted at 35 weeks of gestation due to pain in the right abdomen with 2 weeks of evolution. On admission: hemodynamically stable with tenderness on the right quadrants of the abdomen. The initial blood work only revealed thrombocytopenia (120 × 103/μl) and impaired hepatic function (AST 65 U/L, ALT 88 U/L). The patient was kept on observation, with aggravation of symptoms. Blood work showed anemia (6.9 g/dl), thrombocytopenia (113 × 103/μl) and impaired hepatic function (AST 363 U/L, ALT 399 U/L, LDH 505 U/L). The patient underwent an emergency c-section, during which an extensive hemoperitoneum was observed. It was then converted to median laparotomy in which was observed hepatic rupture of segments V, VI and VII; packing was performed and the abdomen closed. A second-look laparotomy was performed 48 hours later. Two new subcapsular hematomas were found in the left lobe, but without active hemorrhage, which led to the removal of the packing (Figs 3–5).


The patient recovered without complications and was discharged on the 13th postoperative day (Fig. 6).

DISCUSSION
These are two very different cases in terms of clinical presentation and approach. Regarding the first case, the condition developed during labor at 38 weeks of gestation and at 35 weeks of gestation in the second, which required the induction of labor.
As for clinical presentation, abdominal pain is the main manifestation. In the first case, the pain is sudden, whereas in the second it is more insidious, reflecting the heterogeneity and clinical variability of this syndrome.
The blood work results of both patients met the HELLP syndrome criteria, although the second case did not meet initially. Accordingly, the failure to meet all the criteria for HELLP syndrome should not be considered an exclusion factor.
In both cases, the diagnosis was intraoperative and was made during the emergency c-section, following the observation of a massive hemoperitoneum, which led to immediate median laparotomy. This is a rare non-specific pathology, whose diagnosis was made at a late stage, during the intraoperative period.
As far as the surgical approach is concerned, an immediate hepatic packing was performed in both patients. However, it was not possible to fully control the hemorrhage in the first patient, so a Vicryl® prosthesis was placed, commonly used in post-traumatic splenic lacerations. It was adapted ‘in situ’ to this particular situation to cover the entire left lobe of the liver. This is an uncommon approach according to the literature. It is mainly described in the context of trauma surgery as a life-saving measure.
Both patients registered a favorable postoperative course
Hepatic rupture in HELLP syndrome is extremely rare. However, given its sudden and potentially lethal evolution, it is one of the most feared complications and the leading cause of death. A high level of suspicion and early diagnosis are fundamental in the approach to these patients. However, surgeons often encounter an unexpected intraoperative diagnosis as illustrated by the cases above described, requiring a swift and effective intervention. Management is similar to that applied to traumatic lesions of the liver, with the particularity of the hepatic tissue being congested, friable and evidencing associated coagulopathy. The best approach is carried out through median laparotomy and surgical management should be simple and fast according to damage control principles.
CONFLICT OF INTEREST STATEMENT
None declared.



