-
PDF
- Split View
-
Views
-
Cite
Cite
Andreea Bente, Moussa Ouedraogo, Kinjal N Kasbawala, Kristen M Glasgow, Compression of cystic duct caused by focal nodular hyperplasia, Journal of Surgical Case Reports, Volume 2019, Issue 10, October 2019, rjz254, https://doi.org/10.1093/jscr/rjz254
Close - Share Icon Share
Abstract
A 29-year-old female presenting with symptoms of biliary colic was found to have a liver mass compressing the cystic duct. Due to the anatomical placement of the growth, the compressed duct produced symptoms mimicking acute cholecystitis. The mass was diagnosed as focal nodular hyperplasia (FNH) upon biopsy. FNH is commonly found incidentally with nonhepatic clinical presentation or during an unrelated surgical procedure. The scope of this paper is to bring awareness to uncommon causes of biliary colic. To our knowledge, there has been one other paper published with FNH being the primary cause of biliary colic.
INTRODUCTION
An extensive list of diagnostic differentials can be generated from the single chief complaint of “right upper quadrant (RUQ) pain”. Amongst these, gallbladder disease predominates, especially when combined with findings such as postprandial pain, nausea, vomiting and fever. Generally, when gallbladder disease is suspected, it is confirmed with diagnostic imaging and laboratory findings. In the case of inconsistent findings, other rare causes of biliary colic should be suspected, such as external compression from surrounding anatomical structures as presented here.
CASE REPORT
A 29-year-old female with no remarkable past medical history other than a Mirena intrauterine device, presented to the emergency department (ED) with nausea, vomiting and persistent epigastric pain radiating to her RUQ, which occurred in the middle of the night. She had no postprandial pain. Her ultrasound revealed a small amount of biliary sludge, but no signs of acute cholecystitis.
An upper endoscopy was performed to rule out gastritis and ulcerative disease. No remarkable findings were noted during the endoscopy. Lastly, a hepatobiliary HIDA scan with cholecystokinin was obtained which showed normal uptake and drainage with an ejection fraction of 63%.
Considering that biliary sludge was the only finding with further investigation, she was diagnosed with possible biliary colic. However, her unusual symptomatic presentation and consistent RUQ pain suggested the possibility of a different cause. Laparoscopic cholecystectomy was performed. Upon entry into the abdomen, the gallbladder was retracted and a mass on the liver was noted to lie just over the cystic duct (see Fig. 1). The gallbladder was removed in standard fashion with aspiration of only bile from the gallbladder. A biopsy of the liver mass and the gallbladder was sent to pathology.
| Author . | Year . | Gender . | Age . | Type of liver mass . | Symptoms . | Benign or malignant . |
|---|---|---|---|---|---|---|
| Bilanovic | 2008 | Female | 31 | Granular cell tumor | Jaundice, pruritus | Benign |
| Siriwardana | 2009 | Female | 25 | Intrahepatic biliary cystadenoma | Right hypochondriac pain, biliary obstruction | Benign |
| Al Shehri | 2010 | Female | 10 | FNH | Epigastric pain | Benign |
| Kaneya | 2011 | Female | 60 | Simple hepatic cyst | Nontender mass in RUQ | Benign |
| Yano | 2015 | Female | 83 | Hemangioma at hepatic hilar region | Bile duct dilation, obstructive jaundice | Benign |
| Author . | Year . | Gender . | Age . | Type of liver mass . | Symptoms . | Benign or malignant . |
|---|---|---|---|---|---|---|
| Bilanovic | 2008 | Female | 31 | Granular cell tumor | Jaundice, pruritus | Benign |
| Siriwardana | 2009 | Female | 25 | Intrahepatic biliary cystadenoma | Right hypochondriac pain, biliary obstruction | Benign |
| Al Shehri | 2010 | Female | 10 | FNH | Epigastric pain | Benign |
| Kaneya | 2011 | Female | 60 | Simple hepatic cyst | Nontender mass in RUQ | Benign |
| Yano | 2015 | Female | 83 | Hemangioma at hepatic hilar region | Bile duct dilation, obstructive jaundice | Benign |
| Author . | Year . | Gender . | Age . | Type of liver mass . | Symptoms . | Benign or malignant . |
|---|---|---|---|---|---|---|
| Bilanovic | 2008 | Female | 31 | Granular cell tumor | Jaundice, pruritus | Benign |
| Siriwardana | 2009 | Female | 25 | Intrahepatic biliary cystadenoma | Right hypochondriac pain, biliary obstruction | Benign |
| Al Shehri | 2010 | Female | 10 | FNH | Epigastric pain | Benign |
| Kaneya | 2011 | Female | 60 | Simple hepatic cyst | Nontender mass in RUQ | Benign |
| Yano | 2015 | Female | 83 | Hemangioma at hepatic hilar region | Bile duct dilation, obstructive jaundice | Benign |
| Author . | Year . | Gender . | Age . | Type of liver mass . | Symptoms . | Benign or malignant . |
|---|---|---|---|---|---|---|
| Bilanovic | 2008 | Female | 31 | Granular cell tumor | Jaundice, pruritus | Benign |
| Siriwardana | 2009 | Female | 25 | Intrahepatic biliary cystadenoma | Right hypochondriac pain, biliary obstruction | Benign |
| Al Shehri | 2010 | Female | 10 | FNH | Epigastric pain | Benign |
| Kaneya | 2011 | Female | 60 | Simple hepatic cyst | Nontender mass in RUQ | Benign |
| Yano | 2015 | Female | 83 | Hemangioma at hepatic hilar region | Bile duct dilation, obstructive jaundice | Benign |
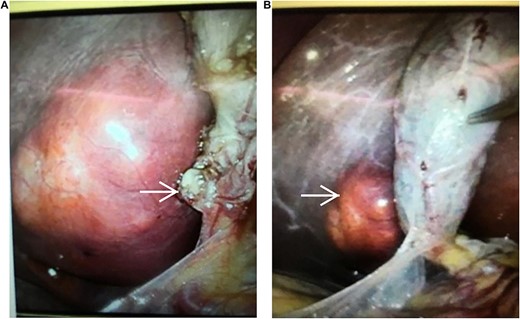
(A, B) The right liver lobe mass (nodular, soft, fatty appearance) compressing cystic duct (arrows), seen during laparoscopic cholecystectomy.
The pathology report revealed chronic cholecystitis with only two 3 mm stones noted and no sludge. The liver biopsy suggested either FNH or hepatocellular adenoma, with the histology being more consistent with FNH findings. The mass was later verified as FNH by the surgical oncologist via MRI.
DISCUSSION
The novelty of this case report lies in the coincidental anatomic placement of the FNH mass, producing an unusual case of RUQ pain. We believe this was the primary contributor to the patient’s chronic cholecystitis as the two gallstones noted were very small to cause her symptoms. Given that her pain occurred while the patient was sleeping, and not postprandial, it is hypothesized that the mass may have been compressing the cystic duct when she was lying down at night. A review of the literature revealed only five other cases with similar presentation due to benign liver mass compression, one of which was found to be focal nodular hyperplasia (FNH).
FNH is a benign liver tumor, commonly diagnosed in young women between 20 and 50 years of age [1]. Usually this mass is detected incidentally, as is the case with the patient in this study. The pathogenesis of FNH has been attributed to abnormal blood to the liver parenchyma due to vessel malformations. The development of the collagenous fibrous scar is due to the over-activation of the transformation growth factor pathway [2, 3]. In few cases, abnormalities can lead to increased angiopoietin 1 and 2, both responsible for blood vessel formation during angiogenesis [2, 3].
There is some conflicting evidence suggesting that women taking oral contraceptive pills (OCPs) are at increased risk for liver masses such as hepatic adenoma and FNH. However, this association is weak especially for patients with a levonorgestrel-releasing contraceptive device, which acts only on progesterone receptors, as was the case with this patient. One study analyzing the effect of combined OCPs found that there was no progesterone receptor expression in FNH biopsy specimens [4].
In search of similar cases of cholecystitis secondary to liver compression, the following PubMed MESH terms were used: cholecystitis, liver mass, FNH and compression (Table 1). Only one case report was found that was similar to our case based on incidental discovery of FNH in the presence of cholecystitis. Al Shehri [6] reported a 10-year-old female with epigastric pain who was found to have acute cholecystitis associated with FNH. Other studies reported various liver masses compressing the common hepatic duct and resulting in symptoms of obstructive jaundice, abdominal pain, elevated alkaline phosphatase and cholecystitis. These include compression of the duct by a granular cell tumor, liver hemangioma and hepatic cyst.
The current case brings to attention an unusual case of RUQ pain which, while rare, warrants consideration for external sources of bile duct compression.
ACKNOWLEDGEMENTS
Dr N. Atweh, Dr W. Cholewczynski, Dr R. Crombie, Dr S. Gregg, Dr A. Savetamal and Dr J. William Tyson.
CONFLICT OF INTEREST
None declared.



