-
PDF
- Split View
-
Views
-
Cite
Cite
William T McSweeney, Kimberley Tan, Cutaneous metastases as a presenting sign of metastatic NSCLC, Journal of Surgical Case Reports, Volume 2019, Issue 10, October 2019, rjz279, https://doi.org/10.1093/jscr/rjz279
Close - Share Icon Share
Abstract
Cutaneous metastases are rare and often late signs of an internal malignancy; however, this can be the presenting sign in very rare cases. These typically have a characteristic appearance and distribution based on the underlying malignancy but can be difficult to distinguish from other malignant or benign dermatoses. We report a case of a 69-year-old female who presented for elective excision of two cutaneous, fast-growing lesions on the chest wall. The patient’s past medical history is significant for a 45-pack-year smoking history. Pre-operative chest radiograph revealed a right upper lobe mass, with the lesions ultimately representing cutaneous metastases of a non-small-cell lung cancer. Although cutaneous metastases have been reported, difficulty remains in distinguishing other causes of cutaneous lesions from cutaneous metastases in the predominantly asymptomatic patient.
INTRODUCTION
Cutaneous metastases are rare sites of metastasis, with an incidence of 5.3% [1]. Whilst the most common internal malignancy overall remains breast cancer, 1–12% of patients with lung cancer may develop cutaneous metastases [2, 3]. The presence of a firm, rapidly growing papular or nodular lesion should prompt the clinician to maintain suspicion of internal malignancy. Whilst lung cancer tends to metastasize to the liver, adrenals, bone and brain, the skin in the supradiaphragmatic region is reported to be the most common location of a cutaneous metastasis [4, 5]. The presence of cutaneous metastases is a poor prognostic factor, often associated with advanced underlying disease and late diagnosis [6]. However, this can rarely be the presenting sign of internal malignancy. Other primary sites of origin of cutaneous metastases include melanoma, as well as breast, ovarian and colorectal cancer [6].
CASE REPORT
A 69-year-old female presented to the general surgical outpatients department on referral from her general practitioner for elective excision of a rapidly growing lesion on her central chest. The lesions had been present for 2 months duration and had increased in size, as well as elevation. They were approximately 5 × 5 × 5 cm and 3 × 3 × 3 cm in size and polypoid in nature, appearing well-circumscribed with a red-purple discoloration, and both had a central depression with ulceration (Fig. 1). The patient was a lifelong smoker (45 pack-year history).

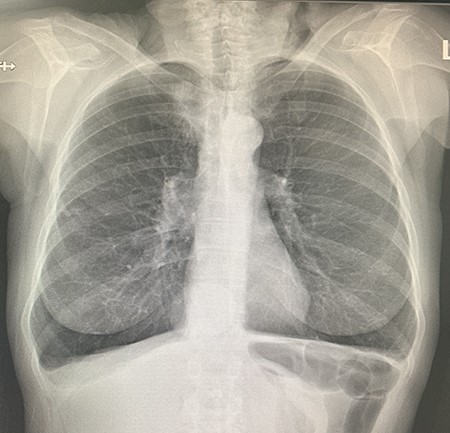
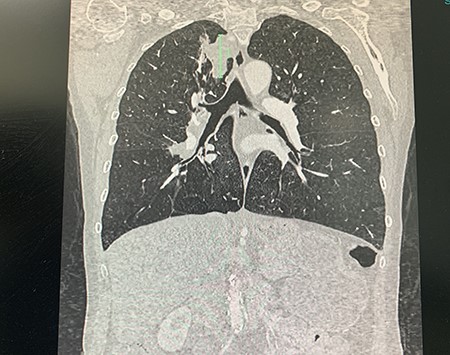
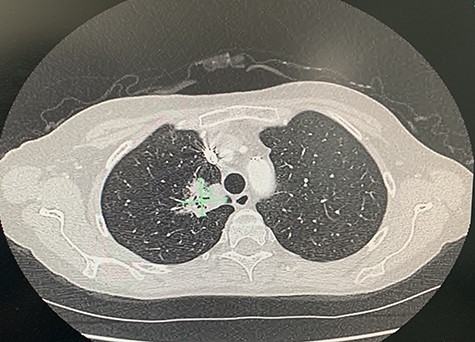
She presented to the operating theatre for excision with incidental dyspnoea and coryzal symptoms, and a pre-operative chest X-ray was arranged before any anaesthetic was administered, revealing a right upper lobe pulmonary mass partly obscured by the clavicle. She underwent excision of the cutaneous lesions, and respiratory physicians were consulted (Fig. 2). Urgent computed tomography (CT) chest was arranged, which revealed the diagnosis of lung malignancy, with a spiculating right apical mass measuring 48 × 30 × 29 mm, extending to the mediastinal pleura and in proximity to the oesophagus and posterolateral trachea with obliteration of the fat planes. There was also local hilar and paratracheal lymphadenopathy, measuring 30 × 29 × 20 mm in the right superior hilar region, 21 × 24 × 13 mm in the right inferolateral hilar region and a 36 × 14 mm pretracheal node (Figs 3 and 4). There were also background mild centrilobular emphysematous changes. There was no metastatic abdominal or pelvic disease.
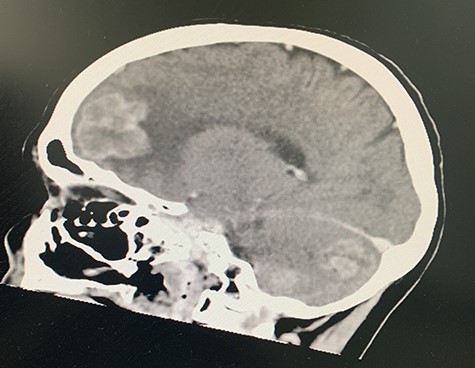
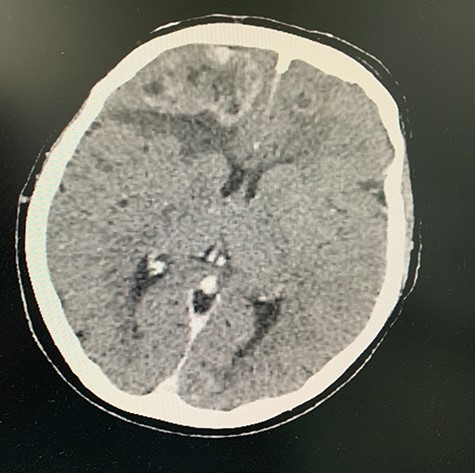
She was referred for urgent respiratory review and discussed at the respiratory Multidisciplinary team (MDT) meeting at a regional referral centre, where staging CT brain revealed six cerebral metastases with two large regions of vasogenic oedema. The metastases were bilateral, but more marked on the right, with the largest lesion in the anteroinferior right frontal lobe producing mass effect on the right lateral ventricle frontal horn and midline shift to the left of 5 mm (Figs 5 and 6). Staging bone scan revealed no bony metastases.
Excision of the skin lesions was carried out with 5 mm margins, with no indication of these lesions being representative of metastases at the time. Histology subsequently revealed poorly-differentiated squamous cell carcinoma, involving some of the margins for both lesions. A supplementary report was issued after the pathologist was notified of the pulmonary mass and clinical context after multidisciplinary meeting, with the tumour cells being positive for GATA-3 and cytokeratin AE1/AE3 and, however, negative for squamous markers. Given that GATA-3 positivity can be seen in 5–10% of lung carcinomas, correlation with the clinical context and radiological findings was suggestive that the lesions represent metastatic lung carcinoma (non-small-cell lung cancer [NSCLC]). Ultimately, the only available pathological diagnosis is one of NSCLC, as squamous markers (p63, CK5/6, TTF-1, Napsin) were all negative and GATA-3 positivity can be found in both squamous cell carcinoma and adenocarcinoma of the lung. The pathologist made a final comment that overall, the tumour could only be determined to be a poorly differentiated carcinoma and that immunohistochemistry (IHC) studies proved unsuccessful in this case in determining a particular histological subtype. Further additional immunohistochemistry revealed estimated glomerular filtration rate BRAF mutation detected (54%), again in keeping with a potential NSCLC.
She was subsequently referred for the initiation of chemotherapy and local radiotherapy. Given the clinical context and current chemoradiotherapy, she has not been booked for any re-excision of margins of these lesions and has been discharged to the care of the respiratory physicians.
Even when considering the rarity of cutaneous metastases, as well as the fact that squamous cell carcinoma (SCC) is not the most common histological subtype to metastasize to the skin, the case represents a significant example of the importance of holistic assessment of the patient, considering risk factors and the clinical context. The chest X-ray provided the initial ‘clue’ into the potential for lesions here to be considered as metastases; indeed even after initial histopathology returned there were alterations made when the clinical context was updated. When considering the indication for procedure, the patient risk factors and the concomitant symptomatology presenting here in the anaesthetic bay, this case highlights the importance of comprehensive and pertinent communication between the surgical team and the histopathologist to ensure that the clinical context is the priority when interpreting results. Obviously, a high index of clinical suspicion is required to reliably diagnose skin metastases [6].
DISCUSSION
Lung malignancy is one of the most common malignancies, with a high rate of mortality [2–4]. The more common locations tend to be hilar nodal involvement, liver, adrenals, bone and brain. But in a small subset of patients, skin metastases can develop with varying rates of between 1 and 12% [4, 5]. Interestingly, when considering a patient with skin metastases, the most common primary site tends to be melanoma for men followed by lung, but falls behind breast, colorectal and ovarian cancer, as well as melanoma in women. Skin metastases tend to portend an aggressive clinical course and can be either synchronous with the underlying malignancy or the sign of recurrence [6].
When skin metastases do occur, the chest and abdomen are the most common site, and they often present as ovoid or round nodules, firm and can be red, dark-red or black. They can also progress to ulceration [7].
Of clinical significance, the presence of cutaneous metastases in this patient group is a poor prognostic indicator, with a reduction of survival to 3 months when coexisting with other metastases [5].
There does appear to be some predilection of location to the supradiaphragmatic region for lung cancers and a higher rate of skin metastases for upper lobe malignancies [4, 5].
Whilst adenocarcinoma histological subtype is the most common type to metastasize to the skin, Squamous cell carcinoma (SCC) is the second most-likely [4].
Pathogenesis is suggested to be by lymphovascular invasion, with poor differentiation and upper lobe tumours increasing the risk [8]. Some suggest that the nodular appearance, that may ulcerate, is more commonly the result of haematogenous spread [5].
Whilst panels for immunohistochemistry can be supportive, they are no substitute for what is described as the ‘big-picture’ approach, when considering these patients and the likely primary site. Data supporting gene mutation analysis in lung cancer patients with cutaneous metastatic disease are lacking [5].
AUTHOR CONTRIBUTIONS
W.T.M. contributed to the conception and design of the study. K.T. contributed to the critical revision of the study and drafting. All authors read and approved the final version of the manuscript.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
ETHICAL APPROVAL
An informed written consent was obtained from the patient.



