-
PDF
- Split View
-
Views
-
Cite
Cite
Maidah Algarni, Enas Raml, Nora Trabulsi, Mohammed Nassif, Small bowel intussusception and concurrent sigmoid polyp with malignant transformation in Peutz–Jeghers syndrome, Journal of Surgical Case Reports, Volume 2019, Issue 1, January 2019, rjz004, https://doi.org/10.1093/jscr/rjz004
Close - Share Icon Share
Abstract
Peutz–Jeghers syndrome (PJS) is an autosomal dominant condition characterized by the association of gastrointestinal polyposis, mucocutaneous pigmentation and cancer predisposition McGarrity, Amos, Baker (Peutz–Jeghers Syndrome, GeneReviews(R), National Center of Biotechnology Information.). Intussusception and malignant polyps are not rare complications of PJS, where the lifetime risk of intussusception is 48% and the possibility of developing any cancer by age 65 years is 37% Kopacova, Tacheci, Rejchrt, Bures (Peutz-Jeghers syndrome: diagnostic and therapeutic approach. World J Gastroenterol 2009;15:5397–408.). Very few cases of malignant polyps causing intussusception associated with synchronous malignant polyp in PJS have been reported to date Cai, Tian, Zhou, He, Hu, Deng (Jejunal intussusception and polyps with different types of malignant transformation in Peutz-Jeghers syndrome: report of a case. Oncol Lett 2013;5:239–41.). We describe a case of a patient with PJS presenting with symptomatic jejunal intussusception and an incidentally found malignant hamartoma in the sigmoid colon.
INTRODUCTION
Peutz–Jeghers syndrome (PJS) is a well-known familial hamartomatous polyposis syndrome, with an incidence of 1 in 8300 to 1 in 280 000 of individuals. PJS predisposes patients to various malignancies such as gastrointestinal, pancreatic, lung, breast, uterine, ovarian and testicular tumors [3]. Hamartomatous polyps mainly found in the small intestine (in order of prevalence: jejunum, ileum and duodenum, respectively), stomach and large bowel [2]. It can also be found in extraintestinal sites including the renal pelvis, bronchus, gall bladder, nasal passages, urinary bladder and ureters [1]. Complications of gastrointestinal polyps include bleeding and intussusception requiring repeated laparotomies and bowel resections [1].
CASE REPORT
A previously healthy 21-year-old male presented to the emergency room with a 2 days history of increasing colicky abdominal pain mainly in the epigastric area. This pain was associated with nausea, vomiting and bloody diarrhea. He had no recent weight loss and no family history of bowel disease.
Upon examination, the patient was afebrile, he had a tender abdomen with no peritoneal signs nor adenopathy. The patient’s skin, including the perioral area, appeared normal, as did the oral mucosa. Laboratory tests indicated low hemoglobin levels, high white blood count, with normal liver and renal function. A contrast enhanced computed tomography (CT) imaging of the abdomen revealed a long segment of jejunal intussusception and a filling defect in the second part of the duodenum, with right side hydroureter and hydronephrosis.
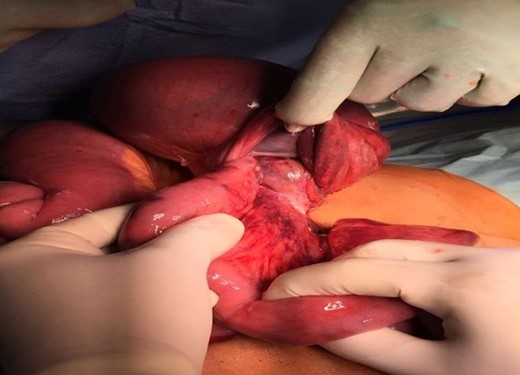
Patient was consented for an exploratory laparotomy and taken to the operating room. During his surgery, a long segment of the proximal jejunum (67 cm) was found to be invaginated into a distal jejunal segment, which confirmed the diagnosis of intussusception (Fig. 1). A mass of 6 cm could be felt at the lead point of the intussusception and the invaginated loop of bowel appeared to be compromised requiring resection of the diseased segment that contains the leading intramural polyp. Careful exploration of the rest of the abdominal cavity and intestine was done, and two additional masses were felt to be tethered inside the sigmoid colon. The sigmoid was redundant and easily resected with good oncological margins (Fig. 2). Giving the patient’s young age, appendectomy was performed as well.

Patient had an uneventful postoperative hospital stay and discharged on fourth day postoperative.
Histopathology showed multiple polyps in the jejunal segment that exhibited features of PJS. These hamartomatous cauliflower-like pedunculated polyps ranged from 0.5 to 3.5 cm in size. The sigmoid mass showed a larger hamartomatous polyps 3.5 × 3.5 × 3 cm3 with low grade dysplasia while some of the jejunal polyps showed transmural infarction.
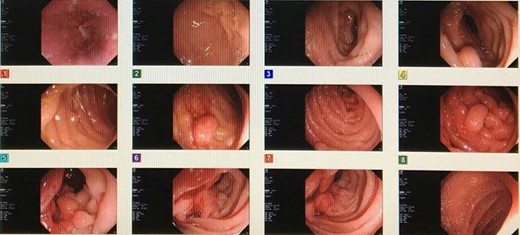
His postoperative upper and lower endoscopy showed numerous diminutive polyps in the gastric fundus and gastric body. It also showed multiple duodenal polyps (3–5 mm) with the largest found at the second part of duodenum involving the ampulla. These were excised and showed normal mucosa with no active or chronic inflammation, atypia or malignancy (Fig. 3) and was booked for follow up endoscopy after 1 year.
DISCUSSION
PJS is an uncommon autosomal dominant inherited disease characterized by the occurrence of hamartomatous polyps in the gastrointestinal tract and mucocutaneous pigmentation. The cause of PJS appears to be a germline mutation of the STK11/LKB1 (serine/threonine kinase 11) tumor suppressor gene located on 19p13.3. This mutation has been found to be primarily responsible for the disease in most cases [4, 5].
Gene testing is not necessary to diagnose PJS but the WHO requires one of the following criteria for diagnosis:
≥3 Hamartomatous polyps;
hamartomatous polyps and a family history of PJS;
mucocutaneous pigmentation and a family history of PJS; and
mucocutaneous pigmentation and hamartomatous polyps [6].
Recently, different diagnostic techniques have been added to the traditional small bowel follow-through and enteroclysis, to assess for small bowel polyps. These include wireless capsule endoscopy, MRI enterography and balloon assisted enteroscopy which could be therapeutic as well [7].
Management of PJS differ according to the presentation, if a polyp discovered upon regular examination by endoscopy and imaging studies, prophylactic endoscopic polypectomy of polyps more than 1 cm is performed. The goal is to decrease the sequelae of large polyps including bleeding, anemia, obstruction, intussusception and malignant transformation [1]. Upper and lower endoscopic examinations are recommended every 3 years, beginning from the age of 18 [8].
CONCLUSION
PJS has the potential for malignant transformation, careful examination of the whole bowel by palpation upon laparotomy should be done. Close follow up and screening with upper and lower endoscopy improves the prognosis and prevents the patient from having repeated surgeries.
ACKNOWLEDGEMENTS
King Abdelaziz University Hospital, Department of General Surgery for the all support.
ETHICS APPROVAL
King Abdul-Aziz University ethical committee has approved this study, consent has been taken from the patient.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.
AUTHORS’ CONTRIBUTIONS
M.A. and E.R. carried out the case presentation, literature review and draft of the discussion, M.N. participated in draft design and review abstract, N.T. carried out draft and design abstract. All authors read and approved the final article.
FUNDING
There is no fund for this case report.



