-
PDF
- Split View
-
Views
-
Cite
Cite
Andrew Jones, Steven Livesey, A novel case of late left ventricular outflow tract obstruction post mitral valve surgery, Journal of Surgical Case Reports, Volume 2019, Issue 1, January 2019, rjy357, https://doi.org/10.1093/jscr/rjy357
Close - Share Icon Share
Abstract
Left ventricular outflow tract (LVOT) obstruction (LVOTO) is a rare but recognized complication of mitral valve surgery. Concomitant factors can cause significant clinical deterioration which requires urgent intervention. We present the case of a female patient who underwent closed valvotomy at age 20 for mitral stenosis secondary to rheumatic heart disease. Seventeen years later, a re-stenosed valve prompted mitral valve replacement (MVR) with a Carbomedics mechanical prosthesis. 8 years later, she re-presented with increasing dyspnoea. On echocardiogram a frond-like structure was visible in the LVOT, the valve housing was protruding into the LVOT and she had marked septal hypertrophy. The LVOT gradient was 72 mmHg. This is a novel case of mechanical MVR associated LVOTO due to at least three discrete factors. This case demonstrates how multiple factors can amalgamate to result in significant clinical deterioration. Over an 8-year period, all three distinct factors contributed to the development of severe LVOTO.
INTRODUCTION
Left ventricular outflow tract (LVOT) obstruction (LVOTO) is a rare but recognized complication of mitral valve surgery. Concomitant factors in patients with an otherwise mild degree of LVOTO can cause significant clinical deterioration which requires urgent intervention. We present a novel case of prosthetic valve associated LVOTO exacerbated by septal hypertrophy and fibrous tissue.
CASE REPORT
We present the case of a 45-year-old female patient with a history of rheumatic fever at the age of 6. At 20 years old, whilst 20 weeks pregnant, she developed crashing pulmonary oedema which responded well to diuretics. Transthoracic echocardiogram (TTE) revealed severe mitral stenosis, with an opening diameter of 10 mm. Due to her age and gestation, a closed valvotomy was performed.
Following that procedure, 17 year later, aged 37 and otherwise fit and well, she had a recurrent episode of pulmonary oedema secondary to re-stenosis of the mitral valve. She underwent mitral valve replacement (MVR) using a 27 mm Carbomedics mechanical valve. Post-operative TTE revealed good left ventricular function and normal function of the mechanical mitral valve.
Then 8 years later, now aged 45, she re-presented with increasing dyspnoea. Of note, she is also now treated for essential hypertension with associated left ventricular hypertrophy (LVH). TTE showed severe LVOTO with a normal appearing prosthetic mitral valve. A frond-like structure was visible in the LVOT and the mechanical valve housing was also protruding into the LVOT. There was some evidence of mitral paravalvular leak as well as left atrial dilatation. Pressure gradient across the LVOT was 72 mmHg.
An urgent re-do MVR was performed. A fibrous band, ~3 mm wide, was found running around the LVOT which was excised using sharp dissection. To further alleviate the gradient across the LVOT, a Morrow resection of the septal shelf was performed. The Carbomedics valve was excised and replaced with a 27 mm St. Jude mechanical valve.
Post-operative TTE showed a dyskinetic interventricular septum with normal left ventricle function otherwise. The outflow tract gradient had reduced to 6 mmHg.
DISCUSSION
LVOTO is a rare but recognized complication following MVR. Factors including the profile of the valve, the aorta-mitral angle and LVH can all contribute to a narrowed LVOT.
There are multiple cases of LVOTO following MVR documented in literature [1]. Many of the cases were due to preserved native leaflets causing LVOTO and systolic anterior motion of the mitral valve [2]. A substantial proportion of the reported literature regarding LVOTO being caused by the prosthesis relates to the struts of bio-prosthetic valves encroaching into the LVOT. Additionally, there were many cases of fibrous material narrowing the LVOT [3].
We believe this to be an interesting and unique case of mechanical MVR associated LVOTO due to at least three discrete factors.
Firstly, the insidious development of left ventricular and septal hypertrophy secondary to hypertension narrowed the LVOT. In a patient with a normal, native mitral valve, this would typically remain subclinical and not manifest any symptoms.
Examining the profile of each valve (Fig. 1), we believe the Carbomedics housing is more predisposed to cause obstruction than the St. Jude. The housing of the Carbomedics prosthesis extends more inferiorly than the St. Jude and potentially into the left ventricular cavity, impinging on the outflow tract. In a patient with coexisting septal hypertrophy, it is clear to see how these two factors alone could cause narrowing. As can be seen in the TTE slice in Fig. 2, the Carbomedics valve is protruding significantly into the LVOT. Severe LVOTO has previously been reported with a Carbomedics mitral valve which was subsequently relieved by replacing the prosthesis with a St. Jude valve [3].

Carbomedics mechanical mitral valve (A) and St. Jude mechanical mitral valve (B) and (C).
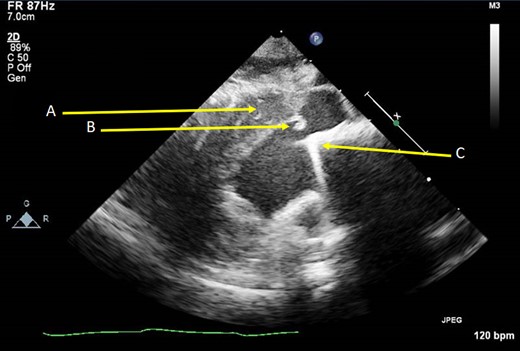
Oblique parasternal long axis TTE image showing thickened IVS (A), subaortic fibrous material (B) and the protruding mitral valve prosthesis (C).
Thirdly, the fibrous band found encircling the LVOT (Fig. 2B) caused further restriction in flow. It is in our opinion that the band will likely have been formed due to turbulent flow from the valve protrusion, though repeated mitral valve prosthesis contact with the interventricular septum has also been shown to cause fibrous material development [4].
CONCLUSION
In the case we have presented here, we demonstrate how multiple concomitant factors can amalgamate to result in significant clinical deterioration. Over an 8-year period, all three distinct factors contributed to the development of severe LVOTO.
CONFLICT OF INTEREST STATEMENT
None declared.



