-
PDF
- Split View
-
Views
-
Cite
Cite
Gabriel Alejandro Molina Proaño, María Mercedes Cobo Andrade, Ramiro Antonio Guadalupe Rodríguez, Patricio Fernando Gálvez Salazar, Diego Paul Cadena Aguirre, Gregorio Vicente González Poma, Bernardo Miguel Gutierrez Granja, Wilkie’s syndrome, a missed opportunity , Journal of Surgical Case Reports, Volume 2018, Issue 9, September 2018, rjy246, https://doi.org/10.1093/jscr/rjy246
Close - Share Icon Share
Abstract
Wilkie’s syndrome is a rare cause of duodenal obstruction that can easily be missed at clinical practice. It is characterized by nausea, abdominal pain and vomit. It usually affects young adults, and it’s caused by a low aortomesenteric angle resulting in vascular compression of the duodenum. Symptoms could resemble many of the symptoms presented in a patient with a suspected eating disorder. The non-specificity of the clinical signs and symptoms can confuse, delay the diagnosis and expose the patient to potentially hazardous therapies. We report a case of a 20-year-old patient who presented to the emergency room with a history of intermittent vomiting and abdominal pain. He had been previously misdiagnosed with an eating disorder and received physiological therapy. Nonetheless, his pain persisted. After further evaluation with the use of imaging techniques, a low aortomesenteric angle was discovered. He underwent surgery and completely recovered. On follow up controls patient is well and he no longer had episodes of vomiting.
INTRODUCTION
Superior mesenteric artery (SMA) syndrome or Wilkie’s syndrome is a rare gastrointestinal disorder present in 0.013–0.3% of the general population [1]. It is characterized by the vascular compression of the duodenum between the aorta and the SMA. This results in partial or total small bowel obstruction [2]. Weight loss and its associated retroperitoneal fatty tissue reduction are thought to be the main cause of this condition. Patients usually present with a history of intermittent vomiting, nausea and abdominal complaints related to the grade of duodenal compression. Symptoms are very vague and can resemble other medical or psychological disorders including eating disorders as anorexia and bulimia [3–5]. We present a case of a 20-year-old male patient, he presented to the emergency room with a history of intermittent vomiting and abdominal pain. He was previously misdiagnosed with an eating disorder and received therapy. Nonetheless, after a CT scan, Wilkie’s syndrome was confirmed. He underwent surgery and completely recovered.
CASE REPORT
A 20-year-old male patient presented to the emergency department with nausea and upper abdominal pain after food intake. His past medical history included an appendectomy, overweight and ~20 kg weight loss in the past 3 years through exercise and dieting. After weight loss, he developed recurrent episodes of vomiting and mild abdominal pain. At that time, vomiting was variable, with episodes occurring once a week to up to three times a day and happened mostly after meals. It was also accompanied by mild depression. Bowel movements were regular and no other symptoms were acknowledged.
With this history, he attended to a physician consultation. Clinical examination was unremarkable, laboratory tests including an upper endoscopy appeared normal at that time. Considering his history and the fact that he had concerns about his body and shape, without any apparent physical dysfunction, an eating disorder was contemplated for which he received 2 years of psychological support. After treatment the vomits and weight loss, to some extent, were controlled. However, he stated that his eating patterns had significantly changed during these years as he mostly ate mushy blended food with liquids; and that even after the treatment pain persisted.
At the time of the assessment in the emergency room, clinical examination revealed dehydration, and abdominal examination revealed periumbilical pain without any tenderness or masses. Laboratory exams revealed anemia and stomach distention was noted on abdominal x-ray. An upper endoscopy was performed revealing a tortuous duodenum in its second and third portions and an extrinsic compression that partially limited the pass of the endoscopy at this point. Due to these findings, surgical consultation was required. A contrast-enhanced CT showed a narrowing at the SMA origin without signs of obstruction (Fig. 1A). An angiotomography with a vascular reconstruction (Fig. 2A) later revealed a 20.5° aortomesenteric angle (Fig. 1B) and 5.26 mm of aortomesenteric distance (Fig. 1C).
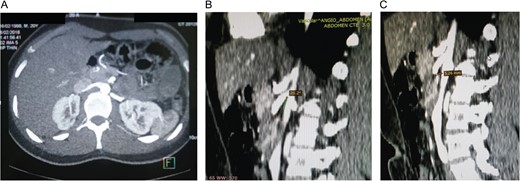
(A) Narrowing at the level of the origin of the superior mesenteric artery without signs of obstruction. (B) Vascular reconstruction showing a 20.5° aortomesenteric angle. (C) Vascular reconstruction showing a closed aortomesenteric angle and a short aortomesenteric distance.
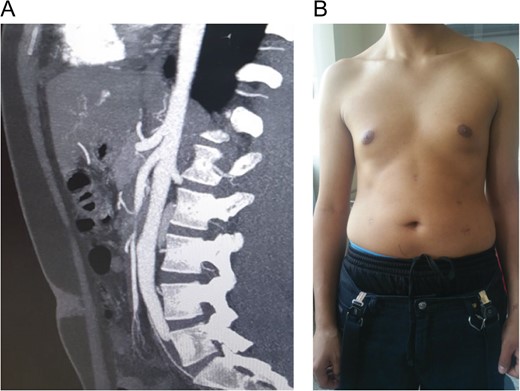
(A) Vascular reconstruction of the patient. (B) Patient 4 months after complete recovery, laparoscopic scars showing on his abdomen.
Wilkie’s syndrome was diagnosed and, given the particularities of this case, a conservative treatment was discarded since the bulimia treatment to gain weight over the last 2 years was not effective. Instead, a surgical treatment was decided.
At laparoscopy, a dilated stomach and duodenum were encountered. The jejunum was identified at the ligament of Treitz, and a segment of jejunum 25 cm distal to the ligament of Treitz was mobilized and attached with a 2-0 absorbable suture to the duodenum. A side to side duodenojejunostomy was performed using a 45-mm linear stapler. The common enterotomy was closed with an absorbable suture without any complications.
From there, the patient had good clinical development. Bowel sound and flatus were present from the third postoperative day and sips of liquids were initiated, attaining good oral tolerance. He was discharged on the seventh postoperative day.
On follow up controls patient is well, 4 months after surgery he started to gain weight (Fig. 2B), and had overcome his depression.
DISCUSSION
Eating disorders are common among teenagers. They are characterized by a loss of control over eating, weight loss by dieting, vomiting, laxative use and excessive exercise. It is suggested that eating disorders may occur due to genetic and physiological influences [3, 4]. When a teenager present with these symptoms, it is not uncommon for a parent to take their child to a physician. When addressing these symptoms in the clinical practice, the possibility of an underlying eating disorder is often considered. However, some patients will have an undiagnosed pathology that could be missed, including Addison disease and Wilkie’s syndrome [6], as was presented in our case. Since Rokitansky first description in 1861, Wilkie’s syndrome is a rare cause of duodenal obstruction [4] caused by the compression of the third portion of the duodenum by the SMA or one of its branches against the aorta [5, 7]. Anatomically, the SMA leaves the aorta at an acute angle that is sustained by adipose tissue, this tissue functions as a natural fatty cushion and prevents extrinsic compression [7]. This obstruction can be; partial or complete; acute or chronic, and congenital or acquired. Short intestinal mesentery, anomalous SMA, high fixation of the duodenum and weight loss (acute or chronic), are among the most common causes. Nevertheless, 40.4% of cases will have no apparent cause [5]. The severity of the symptoms depends mostly on the degree of obstruction [5, 7]. Woman are slightly more affected and mostly occur in young patients between 10 and 39 years [7].
As our patient lost considerable weight, loss of this retroperitoneal fat resulted in a low aortomesenteric angle which in turn caused duodenal obstruction.
Patients usually present with variable and non-specific symptoms including nausea, vomiting and abdominal pain or can present with a long history of intermittent postprandial pain, gastrointestinal discomfort and weight loss [5, 8, 9]. These symptoms can mimic other conditions like pancreatitis, ulcers, eating disorders, etc. and can be aggravated by meals [7, 8]. Diagnosis of Wilkie syndrome is based primary on clinical findings, which makes it challenging and often delayed due to its insidious presentation [8–10]. Imaging is usually necessary. Confirmation is done by computed tomography angiography, which can enable not only the measurement of the aortomesenteric angle and distance, but also the extent of duodenal distension and the amounts of retroperitoneal fat [5].
The treatment will depend on the degree of obstruction. A conservative treatment can be offered at first, which includes some weight gain and the change of some eating habits, which to a certain extent can help relieve the symptoms [6, 7]. When a conservative treatment fails, surgery is usually indicated. Gastrojejunostomy, duodenojejunostomy, or division of the ligament of Treitz could be performed [4]. The use of open and laparoscopic approaches have been previously reported [7, 8], with the latter presenting benefits including shorter hospitalization time and less pain [10]. Clinical suspicion is of most importance, especially in Wilkie syndrome since it has a vague and, in some cases, atypical clinical presentation that could confuse us and delay the diagnosis. Surgeons should always be aware of this rare and often overlooked pathologies, on our daily practice. Misdiagnosis can not only delay treatment, it can expose patients to potentially hazardous therapies. An appropriate history, a physical examination, and complementary tests are of most importance to identify the underlying process of the disease, and define the proper treatment.
CONFLICT OF INTEREST STATEMENT
None declared.



