-
PDF
- Split View
-
Views
-
Cite
Cite
Vinu Perinjelil, Tareq Maraqa, Alex Chavez Yenter, Helen Ohaeri, Leo Mercer, Anish Bansal, Gul Sachwani-Daswani, Traumatic arteriovenous fistula formation secondary to crush injury, Journal of Surgical Case Reports, Volume 2018, Issue 9, September 2018, rjy240, https://doi.org/10.1093/jscr/rjy240
Close - Share Icon Share
Abstract
We describe a patient who suffered a crush injury after a motor vehicle accident leading to complex pelvic injuries complicated by an AV fistula. Traumatic arteriovenous (AV) fistulas from blunt, non-penetrating injuries are uncommon and rarely described in medical literature. A CT followed by pelvic angiogram performed by interventional radiology revealed a traumatic fistula which was then treated by embolization. Patient underwent exploratory laparotomy, craniotomy and open reduction internal fixation of pelvis and was stabilized prior to discharge to rehabilitation.
INTRODUCTION
Arterial injuries can be complicated by the development of arteriovenous fistulas (AVF) which occur as abnormal communications between arteries and veins due to traumatic vessel injury. Few reports record the incidence of traumatic AVF from blunt injuries. Treatment of traumatic fistulas rely on therapeutic combinations of surgical ligation and trans arterial embolization, however this diagnosis can be commonly overlooked if presenting with occult findings. Our case highlights the case of a patient who suffered complex pelvic injuries complicated by a traumatic AV fistula in a motor vehicle accident.
CASE PRESENTATION
An 84-year-old male was brought by EMS to the emergency room due to a crush injury while pinned under a vehicle for nearly 30 min. The patient was conscious with a Glascow Coma Scale (GCS) of 15, breathing spontaneously, with moderate hypothermia (T = 33.4) and hemodynamically unstable (blood pressure = 108/87, heart rate = 88, oxygen saturation = 100). Patient complained of pain and loss of sensation in his right upper extremity and pain throughout the right lower abdomen, back, right hip and right leg. On physical examination, diffuse tenderness was present at the right hip and pelvis and bruising was present on the right groin and bilateral thighs. Patient had an unstable pelvis on physical exam. The clinical picture of hemodynamic instability, hypothermia and pelvic findings indicated a pelvic fracture and pelvic x-ray demonstrated an open book fracture of the pelvis with multiple fractures throughout the pelvic ring (Fig. 1). Pelvic binder was applied. Patient was transported to computed tomography (CT) yet only CT of the head could be performed before the patient became hypotensive. Patient received packed red blood cells (PRBCs) and fresh frozen plasma (FFP) in the trauma bay which responded to blood product resuscitation. Remaining CT scans were completed which revealed chronic subdural hematoma.
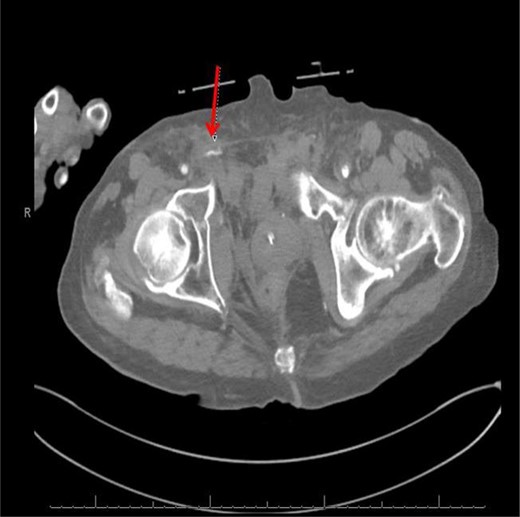
Computed tomography (CT) (axial view) of the abdomen and pelvis demonstrating blush of contrast from distal branch of the right internal iliac artery.
CT abdomen/pelvis with contrast was performed and a blush of contrast was noted posterior to the right pubic bone. Prior to taking patient for exploratory surgery, he was transferred to the interventional radiology suite where a pelvic angiogram was performed revealing an abnormal blush localized to the distal branches of the right iliolumbar artery (Fig. 2). Delayed phase of the angiogram demonstrated early venous filling consistent with a traumatic arteriovenous fistula which was embolized with 300–500 µ of embospheres and three 3 × 2 microcoils (Figs 3 and 4).
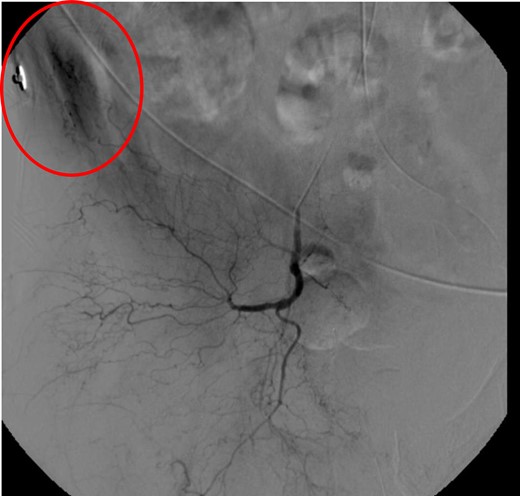
CT angiogram delayed phase of angiogram shows early venous filling consistent with AV fistula.
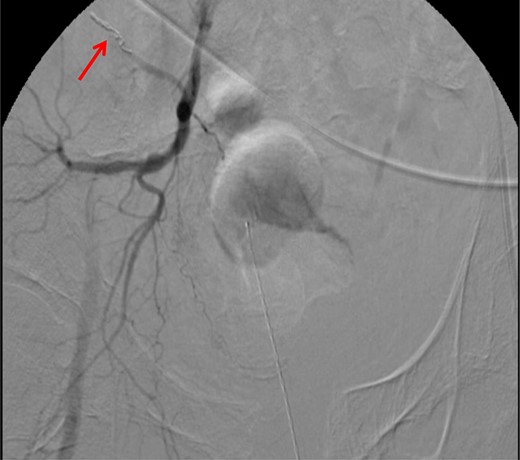
CT angiogram demonstrating microcoil embolization of AV fistula.

CT angiogram demonstrating successful embolization of AV fistula.
After resolution of the traumatic arteriovenous fistula (Fig. 2), a second blush from the right distal internal pudendal artery was identified and successfully treated with Gelfoam slurry. Subsequently, patient underwent exploratory laparotomy which revealed mesenteric and retroperitoneal hematomas. He also underwent craniotomy for evacuation of the subdural hematoma and open reduction internal fixation of the anterior and posterior pelvis. After discharge in fair condition to a subacute rehabilitation facility, patient developed a deep venous thrombosis managed by Coumadin.
DISCUSSION
AVF result in shunting of blood creating a low-resistance and high-flow system which bypasses capillary vasculature and denies tissue perfusion [1]. AV fistulae can be clinically asymptomatic (15%) or present as a machinery murmur with or without palpable thrill (61%) or a pulsatile mass (20%) [2]. Overall, 85% of AV fistulae manifest within 8 weeks of development, and of those ‘late presenters’ who presented after that time, 96% had a machinery murmur [2]. Table 1 shows the time spans from injury to intervention of AV fistulas recorded in literature.
| Associated pelvic injury . | Time span from injury to intervention . | Comments . |
|---|---|---|
| Pubic diastasis, sacral fracture | 4 h | The case presented in this case report, AVF between right iliolumbar artery and vein |
| Separated pubic symphysis, right sacroiliac subluxation [3] | 15 h | Traumatic AV fistula between left internal pudendal artery and vein; |
| Pelvic bone fracture, bulbar urethral lesion [4] | 46 days | Pseudoaneurysm associated with AV fistula connected to Santorini plexus |
| Blunt injury to leg [5] | 3 months | Pseudoaneurysm in left distal superficial femoral artery with fistula connection to femoral vein |
| Severe blunt trauma to left side of pelvis [6] | 1.5 years | Multiple small AV fistulae between left internal iliac artery and vein |
| Pelvic fractures, injury to posterior trunk of internal iliac artery [7] | 13 years | Large AV fistula on posterior trunk of internal iliac artery; 4 years of cardiac failure secondary to AV fistula unresponsive to digitalis and diuretics |
| Iliac bone fracture with post-traumatic heterotopic bone [8] | 20 years | AV fistula between right internal iliac artery and vein at level of sciatic notch; hypertrophy of gluteal muscles, otherwise asymptomatic at time of diagnosis |
| Fracture at the superior and inferior rami of the right pubic bone [9] | No intervention | Right reno-caval AVF, AVF closed spontaneously, but kidney was rendered atrophic and non-functional |
| Associated pelvic injury . | Time span from injury to intervention . | Comments . |
|---|---|---|
| Pubic diastasis, sacral fracture | 4 h | The case presented in this case report, AVF between right iliolumbar artery and vein |
| Separated pubic symphysis, right sacroiliac subluxation [3] | 15 h | Traumatic AV fistula between left internal pudendal artery and vein; |
| Pelvic bone fracture, bulbar urethral lesion [4] | 46 days | Pseudoaneurysm associated with AV fistula connected to Santorini plexus |
| Blunt injury to leg [5] | 3 months | Pseudoaneurysm in left distal superficial femoral artery with fistula connection to femoral vein |
| Severe blunt trauma to left side of pelvis [6] | 1.5 years | Multiple small AV fistulae between left internal iliac artery and vein |
| Pelvic fractures, injury to posterior trunk of internal iliac artery [7] | 13 years | Large AV fistula on posterior trunk of internal iliac artery; 4 years of cardiac failure secondary to AV fistula unresponsive to digitalis and diuretics |
| Iliac bone fracture with post-traumatic heterotopic bone [8] | 20 years | AV fistula between right internal iliac artery and vein at level of sciatic notch; hypertrophy of gluteal muscles, otherwise asymptomatic at time of diagnosis |
| Fracture at the superior and inferior rami of the right pubic bone [9] | No intervention | Right reno-caval AVF, AVF closed spontaneously, but kidney was rendered atrophic and non-functional |
| Associated pelvic injury . | Time span from injury to intervention . | Comments . |
|---|---|---|
| Pubic diastasis, sacral fracture | 4 h | The case presented in this case report, AVF between right iliolumbar artery and vein |
| Separated pubic symphysis, right sacroiliac subluxation [3] | 15 h | Traumatic AV fistula between left internal pudendal artery and vein; |
| Pelvic bone fracture, bulbar urethral lesion [4] | 46 days | Pseudoaneurysm associated with AV fistula connected to Santorini plexus |
| Blunt injury to leg [5] | 3 months | Pseudoaneurysm in left distal superficial femoral artery with fistula connection to femoral vein |
| Severe blunt trauma to left side of pelvis [6] | 1.5 years | Multiple small AV fistulae between left internal iliac artery and vein |
| Pelvic fractures, injury to posterior trunk of internal iliac artery [7] | 13 years | Large AV fistula on posterior trunk of internal iliac artery; 4 years of cardiac failure secondary to AV fistula unresponsive to digitalis and diuretics |
| Iliac bone fracture with post-traumatic heterotopic bone [8] | 20 years | AV fistula between right internal iliac artery and vein at level of sciatic notch; hypertrophy of gluteal muscles, otherwise asymptomatic at time of diagnosis |
| Fracture at the superior and inferior rami of the right pubic bone [9] | No intervention | Right reno-caval AVF, AVF closed spontaneously, but kidney was rendered atrophic and non-functional |
| Associated pelvic injury . | Time span from injury to intervention . | Comments . |
|---|---|---|
| Pubic diastasis, sacral fracture | 4 h | The case presented in this case report, AVF between right iliolumbar artery and vein |
| Separated pubic symphysis, right sacroiliac subluxation [3] | 15 h | Traumatic AV fistula between left internal pudendal artery and vein; |
| Pelvic bone fracture, bulbar urethral lesion [4] | 46 days | Pseudoaneurysm associated with AV fistula connected to Santorini plexus |
| Blunt injury to leg [5] | 3 months | Pseudoaneurysm in left distal superficial femoral artery with fistula connection to femoral vein |
| Severe blunt trauma to left side of pelvis [6] | 1.5 years | Multiple small AV fistulae between left internal iliac artery and vein |
| Pelvic fractures, injury to posterior trunk of internal iliac artery [7] | 13 years | Large AV fistula on posterior trunk of internal iliac artery; 4 years of cardiac failure secondary to AV fistula unresponsive to digitalis and diuretics |
| Iliac bone fracture with post-traumatic heterotopic bone [8] | 20 years | AV fistula between right internal iliac artery and vein at level of sciatic notch; hypertrophy of gluteal muscles, otherwise asymptomatic at time of diagnosis |
| Fracture at the superior and inferior rami of the right pubic bone [9] | No intervention | Right reno-caval AVF, AVF closed spontaneously, but kidney was rendered atrophic and non-functional |
In a study which focused on traumatic AV fistulae in general (n = 202), there was only one reported fistula (0.005%) in the anatomical distribution of the pelvis [2]. More common locations of AV fistula formation were the cervicomediastinal region, upper limb, thorax, abdomen and lower limb. Another study which focused on vascular injuries in general (n = 387) reported traumatic AV fistulae in 5.8% of cases, in contrast to arterial thrombosis, complete and partial vascular rupture and traumatic pseudoaneurysm [3]. This study also showed that pelvic fracture and involvement of the internal iliac artery were both rare occurrences, and we illustrate those rare cases in literature here (Table 2). Our patient had diffuse non-penetrating trauma resulting in vascular, osseous and soft tissue injuries which intersects minorities of both trauma and vascular cases.
| Study focus . | Greater incidence . | Lesser incidence . |
|---|---|---|
| Pelvic trauma [9] | Blunt injuries | Penetrating injuries |
| Acute AV fistulae [2] | Penetrating injuries | 2% Blunt injuries |
| Extra-pelvic locations | 0.005% Pelvic location | |
| Blunt abdominal trauma [4] | Extra-pelvic injuries | 20% with Pelvic fracture |
| Vascular injury [10] | Extra-pelvic fistulae | 5.8% Traumatic AV fistulae |
| Other fracture | 1.8% Pelvic fracture | |
| Other vessel involvement | 0.01% Involvement of internal iliac artery |
| Study focus . | Greater incidence . | Lesser incidence . |
|---|---|---|
| Pelvic trauma [9] | Blunt injuries | Penetrating injuries |
| Acute AV fistulae [2] | Penetrating injuries | 2% Blunt injuries |
| Extra-pelvic locations | 0.005% Pelvic location | |
| Blunt abdominal trauma [4] | Extra-pelvic injuries | 20% with Pelvic fracture |
| Vascular injury [10] | Extra-pelvic fistulae | 5.8% Traumatic AV fistulae |
| Other fracture | 1.8% Pelvic fracture | |
| Other vessel involvement | 0.01% Involvement of internal iliac artery |
| Study focus . | Greater incidence . | Lesser incidence . |
|---|---|---|
| Pelvic trauma [9] | Blunt injuries | Penetrating injuries |
| Acute AV fistulae [2] | Penetrating injuries | 2% Blunt injuries |
| Extra-pelvic locations | 0.005% Pelvic location | |
| Blunt abdominal trauma [4] | Extra-pelvic injuries | 20% with Pelvic fracture |
| Vascular injury [10] | Extra-pelvic fistulae | 5.8% Traumatic AV fistulae |
| Other fracture | 1.8% Pelvic fracture | |
| Other vessel involvement | 0.01% Involvement of internal iliac artery |
| Study focus . | Greater incidence . | Lesser incidence . |
|---|---|---|
| Pelvic trauma [9] | Blunt injuries | Penetrating injuries |
| Acute AV fistulae [2] | Penetrating injuries | 2% Blunt injuries |
| Extra-pelvic locations | 0.005% Pelvic location | |
| Blunt abdominal trauma [4] | Extra-pelvic injuries | 20% with Pelvic fracture |
| Vascular injury [10] | Extra-pelvic fistulae | 5.8% Traumatic AV fistulae |
| Other fracture | 1.8% Pelvic fracture | |
| Other vessel involvement | 0.01% Involvement of internal iliac artery |
While blunt pelvic trauma is more common than penetrating pelvic trauma [4], most causes of acute AV fistulae are penetrating trauma (98%) [2]. Involvement of pelvic injury is as rare as 20% as evidenced in a study by Fitzgerald of 200 abdominal injuries [4]. Furthermore, no reports have documented the incidence of AVF from crush injuries. Crush injuries, a result of compression to the body from objects can lead to systemic manifestations like muscle damage, hemodynamic instability, organ dysfunction and metabolic abnormalities. The need to identify and appropriately treat vascular injuries early even in those with blunt injuries is critical. Sequelae of untreated AV fistulae include hyperdynamic congestive heart failure [2, 5, 6], hemihypertrophy of ipsilateral musculature, lower extremity ulcerations [7], impotence [6], pre-capillary pulmonary artery hypertension [6], dilation of the afferent arteries and efferent veins, with a possible formation of pulsatile varices or venolymphatic trophic complications [7]. If the AV fistula is associated with a pseudoaneurysm, additional complications include thrombosis, embolism, infection and rupture [8].
Current treatments of AVF are embolization, surgery or a combination with preoperative embolization followed within 48 hours by surgery [8]. Traumatic AV fistulas are diagnosed by arteriography for definitive diagnosis, and there is a statistically improved survival rate when transcathether arterial embolization occurs within three hours of arrival to the hospital [9]. An arteriogram consistent with an AV fistula would show early filling of a vein adjacent to a contrast opacified artery, exhibiting a connection between the two vessels [9]. Materials used for embolization in the trauma setting are most commonly coils, microcoils or Gelfoam [9]. In the setting of an AV fistula, coil may be the most appropriate agent as they allow precise embolization [10]. and a combination of coils and Gelfoam can be used if the patient is severely coagulopathic [10]. Complications of AV fistula embolization range from 2 to 11.2% [2, 10] and include recurrent fistulae, repeat bleeding, tissue ischemia, paresthesias, poor wound healing and deep infections [10].
CONFLICT OF INTEREST STATEMENT
None declared.



