-
PDF
- Split View
-
Views
-
Cite
Cite
Shogik Abramyan, Mahmoud W Almadani, Sandeep Sirsi, Philip Q Xiao, Armand P Asarian, Perforation of appendiceal adenocarcinoma ex goblet cell carcinoid: a rare case, Journal of Surgical Case Reports, Volume 2018, Issue 9, September 2018, rjy242, https://doi.org/10.1093/jscr/rjy242
Close - Share Icon Share
Abstract
Goblet cell carcinoid tumor is a rare form of carcinoid tumor of the appendix. It behaves more aggressively than classical carcinoid tumor of the appendix. Thus, special attention must be given to its disease course and treatment. Our case presentation is of a 68-year-old female who presented with abdominal pain. Computed tomography of her abdomen and pelvis showed a perforated appendicitis. She underwent an ileocectomy with pathological report showing a goblet cell carcinoid tumor of the appendix with negative lymph nodes. A subsequent colonoscopy done 5 months later showed no synchronous lesions and a healthy anastomosis. Given the limited amount of data available about goblet cell carcinoid tumors of the appendix, it is important to report all findings in an effort to improve our understanding and treatment approaches of this rare disease.
INTRODUCTION
Goblet cell carcinoid tumor (GCT)—also termed mucinous carcinoid tumor, mixed crypt cell carcinoma, adenocarcinoid–goblet cell type, and microglandular goblet cell carcinoma—is a rare pathology of the appendix, and almost exclusive to the appendix [1]. It contains features of both neuroendocrine neoplasm and glandular adenocarcinoma. As such, it behaves in an intermediate fashion; more aggressively than a classic carcinoid tumor but less so than an adenocarcinoma. In this article, we will present a rare case of a mixed adenocarcinoma ex goblet cell carcinoid tumor found incidentally after an appendectomy.
CASE PRESENTATION
A 68-year-old female presented with complaints of intermittent sharp, cramping abdominal pain for 6 days. She had two days of loose stools prior to presentation. She also reported a decreased appetite in the past week. In the emergency department she had a leukocytosis with a left shift and an acute kidney injury as reflected by her elevated creatinine from baseline. The CT scan of her abdomen and pelvis revealed a perforated appendix with a large abscess collection. The decision was made to take the patient to the operating room. In the operating room, she was found to have a gangrenous appendix and terminal ileum and a 50 ml abscess cavity was drained; thus, an ileocecectomy was done with a subsequent ileocolic primary anastomosis. The post-operative course was uneventful; the patient was discharged on post-operative Day 9.
PATHOLOGY
Microscopic examination reveals thickened appendicial wall with infiltrating individual malignant cells (Fig. 1).
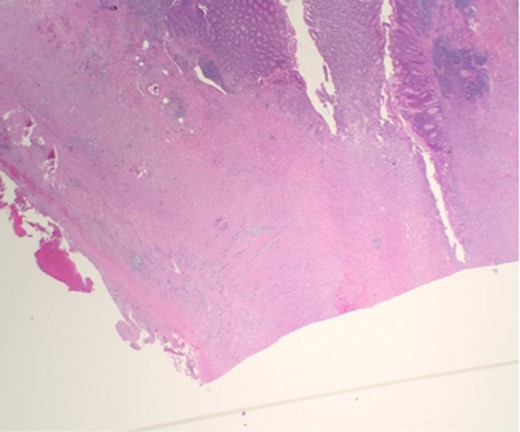
Microscopic examination reveals thickened appendicial wall with infiltrating individual malignant cells.
High-power examination reveals some malignant cells demonstrating Signet ring cell features (Fig. 2).
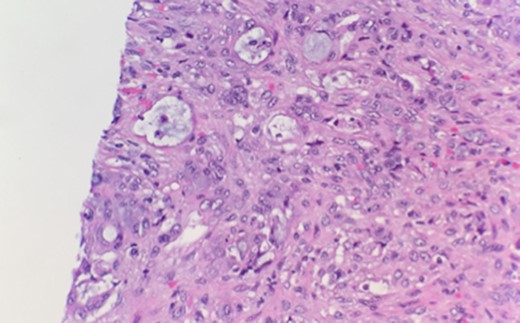
High-power examination reveals some malignant cells demonstrating Signet ring cell features.
DISCUSSION
Goblet cell carcinoid tumors have an intermediate aggressiveness. The disease-specific 5-year survivals for stages I, II, III and IV were 100, 76, 22 and 14%, respectively [2].
Given the rarity of goblet cell carcinoids, standards of care do not exist, and guidelines conflict. Varying guidelines are largely dependent on tumor size, location and spread. Some suggest that simply an appendectomy alone is sufficient for localized cases [3]. Others, for example, the North American Neuroendocrine Tumor Society (NANET) recommends a formal right hemicolectomy in patients found to have appendiceal carcinoids with evidence of tumors >2 cm, incompletely resected tumors, lympho-vascular invasion and mixed histology (goblet cell carcinoid, adenocarcinoid) [4]. According to NANET, appendiceal adeno-carcinoids (goblet cell carcinoids) should be treated like adenocarcinoma rather than a carcinoid tumor [4]. However, the overall 5-year survival rates for patients with combined stages II–IV who underwent appendectomy versus right hemicolectomy were 43 and 34%, respectively [2]. Hence, the optimal treatment remains unclear.
The role of adjuvant chemotherapy also remains controversial. FOLFOX (5FU, leucovorin, oxaloplatin) regimen was used in one study resulting in complete remission [5]. Another study found adjuvant chemotherapy to give no statistically significant improvement in survival rates [2]. In our patient, given that she had a complete resection with negative margins and negative lymph nodes, chemotherapy was no deemed necessary.
Postreatment follow-up is another controversial topic. According to NCCN guidelines for appendiceal NETs ≤2 cm confined to the appendix and treated by simple appendectomy, no follow-up is required. For larger or node-positive tumors, between 3 and 12 months postresection, a history and physical examination, and chromogranin testing is recommended. Beyond 1 year postresection, a history and physical examination every 6–12 months along with chromogranin testing and radiographic imaging studies annually is recommended. Our patient was referred to Mount Sinai for follow up; it was decided that chemotherapy was not beneficial for her. We followed up with her at our institution 5 months after her original surgery for a colonoscopy. Her colonoscopy was uneventful, no synchronous lesions were found, no recurrence was noted, and her anastomosis looked healthy. She will continue to follow up at Mount Sinai for serial physicals and likely radiographic imaging.
Special consideration must be given to cases of perforated appendices, similar to our patient’s presentation. There is no clear connection between recurrence or metastasis in cases of classical appendiceal carcinoid tumor perforation. However, there is a higher risk of peritoneal carcinomatosis among cases of perforated appendiceal goblet cell carcinoid tumors, but the true prognostic impact of perforation on the development of peritoneal carcinomatosis has yet to be determined [6]. Close surveillance is recommended in these cases, especially in female patients as ovarian metastasis has been reported.
CONCLUSION
In conclusion, given its extremely rare nature, goblet cell carcinoid tumor of the appendix remains the least understood subtype of appendiceal carcinoid tumors. Further research is necessary to formulate guidelines for proper surgical treatment approaches and whether or not chemotherapy/radiotherapy are a useful treatment option.
ACKNOWLEDGEMENTS
Not applicable.
CONFLICT OF INTEREST STATEMENT
Not applicable.
DECLARATIONS
No applicable.
AVAILABILITY OF DATA
Not applicable.



