-
PDF
- Split View
-
Views
-
Cite
Cite
Benjamin W Deschner, Steven J Schwulst, Spontaneous reduction of acute cecal herniation through the foramen of Winslow, Journal of Surgical Case Reports, Volume 2018, Issue 9, September 2018, rjy236, https://doi.org/10.1093/jscr/rjy236
Close - Share Icon Share
Abstract
This is the case of a 70-year-old woman who presented to the emergency department complaining of 2 hours of acute-onset epigastric pain. She had experienced this pain once before which had spontaneously resolved. Axial imaging demonstrated the cecum in an abnormal position within the lesser sac, as well as compression of the inferior vena cava and portal vein. She was taken emergently to the operating room for laparotomy, where a free-floating cecum and ascending colon was identified without ischemia, and a right hemicolectomy was performed. Foramen of Winslow hernias are rare internal hernias with a high rate of strangulation and bowel ischemia, requiring urgent surgical intervention. Operative treatment depends on the type of herniated viscera. Spontaneous reduction is not well documented.
INTRODUCTION
The foramen of Winslow (FoW) is a congenital opening between the lesser sac and peritoneal cavity, typically ~3 cm in diameter, bordered anteriorly by the portal triad, posteriorly by the IVC, superiorly by the caudate lobe of the liver, and inferiorly by the duodenum [1]. Herniation of viscera through the FoW was first reported by Bladin in 1834. With <200 cases reported in the literature, these rare hernias are thought to comprise <10% of all abdominal internal hernias. Roughly two-thirds involve herniation of small bowel, with the majority of the remaining cases involving the terminal ileum, cecum and right colon. Rarely, transverse colon and even the gallbladder may be the primary herniated viscera [2]. Predisposing anatomical factors have been identified to be a large FoW, elongated mesentery or mesocolon, abnormally mobile cecum and right colon and anatomy which would predispose ‘funneling’ of the viscera to the foramen (e.g. Reidel’s lobe). An episode of increased intra-abdominal pressure often precedes pain on presentation, suggesting this is the final component in etiology in a patient with such anatomic predispositions [3].
Patient presentation can be quite variable. Vague epigastric pain is often the most consistent complaint, but post-prandial nausea and emesis consistent with a proximal obstruction as well as jaundice may occur given compression of the dilated herniated viscera on the surrounding stomach and common bile duct. Quite often patients may present obstructed and with peritonitis, as the internally herniated contents are ischemic [4]. Diagnosis is most often secured by computed tomography, with imaging findings listed in Table 1 [1, 5]. This case report describes a patient with radiographically evident herniation of the cecum through the FoW, which spontaneously reduced prior to abdominal entry.
|
|
|
|
CASE REPORT
The patient is a 70-year-old woman who presented to the emergency department with acute-onset abdominal pain throughout her epigastrium for approximately 2 hours. The pain was constant and severe, extending across the bilateral upper quadrants. She had experienced pain like this once before within the past year which spontaneously resolved within 4 hours. The patient’s last oral intake was an hour before onset of the pain, and she denied any fevers, chills, nausea or vomiting. She was an otherwise healthy woman who took no medications and had no abdominal surgical history. On admission, vital signs were normal, with a heart rate in the 70’s. Although initially reported as tender by emergency department staff, after pain medication and intravenous fluids, examination by the surgical team revealed resolution of pain and a soft, non-tender abdomen. Lactic acid on presentation was 5.0 mmol/l, and her white blood cell count was 9600 µl−1, with the remainder of her laboratory values within normal limits. She underwent a computed tomography scan which demonstrated herniation of her cecum through the FoW, causing compression of the inferior vena cava (IVC) and portal vein (Figures 1–3).
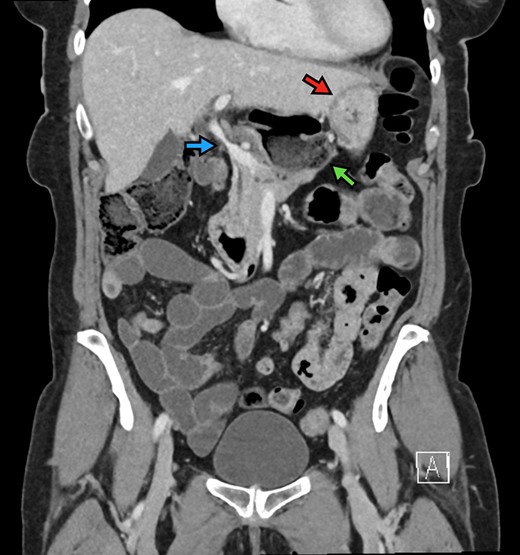
The cecum is absent from the right lower quadrant and is located between the liver and stomach (red arrow) visualized as an air-fluid level (green arrow). Compression of the portal vein by herniated contents is demonstrated (blue arrow).
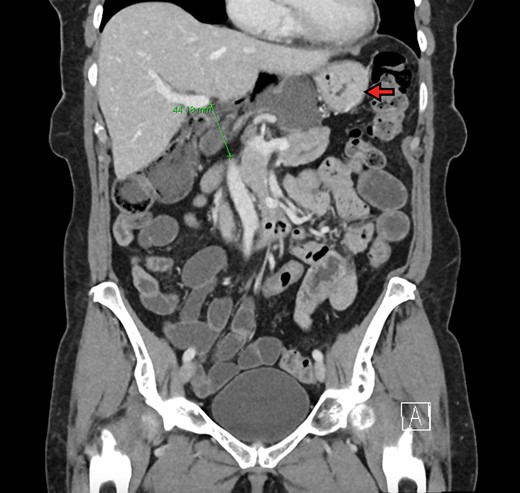
Coronal view demonstrating FoW measurement and herniated contents. The stomach is demonstrated by the red arrow. The FoW is shown to be dilated at 4.4 cm.

Axial view demonstrating multiple air-fluid levels posterior to the liver and adjacent to the stomach (red arrow).
The patient was taken to the operating room for a laparotomy. On exploration, the cecum was found to be free-floating with significant mobility of the right colon mesentery. It appeared to have spontaneously reduced. A right hemicolectomy was performed, resecting all the redundant right-sided colon and creating a primary side-to-side functional end-to-end anastomosis.
Post-operatively, the patient’s presenting pain had resolved, she tolerated rapid advancement of diet, and was discharged once bowel function was regained. She was seen in the outpatient clinic at 2 weeks post-operatively and was doing well without recurrence of symptoms.
DISCUSSION
Herniation through the FoW is a surgical emergency, given the high potential for bowel ischemia and mortality rates ranging from 36 to 49% with a delayed diagnosis [2]. Classically, FoW hernia is approached with laparotomy, although successful laparoscopic intervention has been reported [6]. The surgical principles involved include reducing the hernia, resecting non-viable viscera and performing measures to prevent future occurrences.
Intraoperative reduction can be quite challenging. If initial gentle compression and traction is not sufficient, progressive measures include opening the lesser sac to assist manual reduction, aspirating fluid and air directly from the dilated, herniated loop and eventually performing a Kocher maneuver to enlarge the foramen [4]. In situ resection within the lesser sac rarely need be performed. Resection of non-viable bowel is straight-forward, but the method of preventing recurrences is controversial. Resection and anastomosis of hypermobile bowel (as in our case) has been well described. Pexy of bowel and obliterating the FoW with omentum have also been reported. Many authors report actual safe sutured closure of the FoW; however, obstructive jaundice and portal vein thrombosis are known complications of this technique [7]. Laparoscopic reduction with no preventative intervention has also been performed, and to date no recurrence has ever been reported regardless of practice.
Interestingly, our case demonstrated a FoW hernia convincingly by imaging, but which had spontaneously reduced prior to operation. Spontaneous reduction of internal hernias has been postulated as a source of occult intermittent abdominal pain; however, spontaneous reduction of a radiographically confirmed hernia of the cecum through the FoW is not well-documented. The patient reported here also described a similar episode of pain lasting for several hours months prior to her current presentation, which resolved without intervention.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- ischemia
- gastrointestinal tract vascular insufficiency
- epigastric pain
- emergency service, hospital
- hernias
- laparotomy
- operating room
- pain
- portal vein
- surgical procedures, operative
- inferior vena cava
- cecum
- diagnostic imaging
- viscera
- strangulation
- colectomy, right
- epiploic foramen
- ascending colon
- compression



