-
PDF
- Split View
-
Views
-
Cite
Cite
Raul Caso, Dany Barrak, Taryn E Travis, Laura S Johnson, Jeffrey W Shupp, Survival from a 75% TBSA thermal injury complicated by bowel ischemia presenting with pneumatosis intestinalis, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy235, https://doi.org/10.1093/jscr/rjy235
Close - Share Icon Share
Abstract
Thermal injury is associated with an increased risk of abdominal complications such as ischemia, infarction and pneumatosis intestinalis (PI). PI is characterized by gas in the intestinal wall and, when diagnosed it can signify the presence of a life-threatening condition. We present a case of a patient who survived 75% total body surface area burns complicated by ischemic bowel that initially presented as extensive PI. This patient was emergently taken to the operating room and underwent a subtotal colectomy and small bowel resection for ischemic bowel. Prompt diagnosis and successful management of the underlying condition ultimately contributed to the patient’s survival. The presence of peritonitis or abdominal distension, portomesenteric venous gas and lactic acidosis should prompt immediate surgical intervention in the post-burn period.
INTRODUCTION
Burn patients are at high risk for ischemic enterocolitis (IE) in the immediate post-burn period. If pneumatosis intestinalis (PI) is identified radiographically, diagnostic efforts should attempt to rule out ischemic bowel and necrosis as these carry a high incidence of mortality. PI is a rare condition characterized by gas in the wall of the gastrointestinal (GI) tract [1] with its treatment and prognosis depending on the cause. The true incidence of PI is largely unknown as most patients are asymptomatic. In the burn population, this condition is not well described—perhaps because it largely goes undiagnosed or it is underreported. Here we present a patient with 75% TBSA thermal injury, complicated by bowel ischemia and early evidence of extensive PI, who ultimately survived as a result of prompt diagnosis and surgical management.
CASE REPORT
A 30-year-old woman 34 weeks pregnant was assaulted with an accelerant resulting in burn injuries to her trunk and limbs. Her past medical history was only significant for two prior uncomplicated cesarean sections. We chronicle the care of this patient from admission to discharge in Fig. 1. Upon arrival to the Burn Center, her primary survey was significant for tachycardia with a heart rate of 134 bpm. Otherwise, she was breathing spontaneously and had an adequate airway; her first recorded blood pressure was 136/64, and her GCS was 15. Total burn area was calculated to be 75% TBSA (deep partial- and full-thickness). Her abdomen was gravid, but a bedside ultrasound showed no fetal cardiac motion. The patient was intubated and an emergent cesarean section was performed via a midline vertical incision. The child was delivered with APGAR scores of 1/5/6 at 1/5/10 min. The hysterotomy was subsequently closed in the standard fashion, the abdomen was irrigated with warm saline, and fascia was closed.
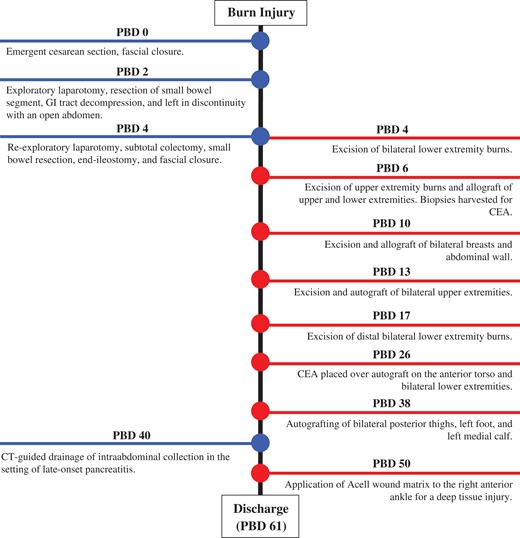
Timeline of care from admission to discharge. (Abbreviations: PBD, post-burn day; PI, pneumatosis intestinalis; HPVG, hepatic portal venous gas; CT, computed tomography; GI, gastrointestinal; CEA, cultured epithelial autograft.)
Intravenous fluid resuscitation with lactated Ringer’s (LR) was initiated using the Consensus formula, which ultimately totaled 22 L during the first 24 h from burn injury (4 mL/kg/%TBSA). Fresh frozen plasma was used as a colloid adjunct to LR. Laboratory results on arrival were as follows: WBC 25.2 K/uL; Hgb 13.3 g/dL; Hct 40.6%; platelets 506 K/uL. The liver and kidney function indices were all in the normal range. Enteral feeds were initiated within the first 24 h.
On the evening of post-burn day (PBD) 2, the patient developed a distended abdomen and became oliguric, unresponsive to volume challenge. A portable abdominal x-ray was concerning for pneumatosis of the stomach, small bowel and colon (Fig. 2). Computed tomography (CT) confirmed pneumatosis of the esophagus, stomach, small bowel and much of the colon, and hepatic portal venous gas (HPVG)—concerning for ischemic bowel (Fig. 3A–C) and prompting operative intervention. Of note, all vessels were patent. In the operating room (OR), the GI tract was distended with pneumatosis but without signs of ischemia except for a segment of mid-jejunum which was resected. She became hemodynamically unstable and thus left in discontinuity and an open abdomen.

Portable abdominal x-ray significant for pneumatosis of the stomach, small bowel and colon, without evidence of pneumoperitoneum. Note that safety pins visible in the image are external objects.
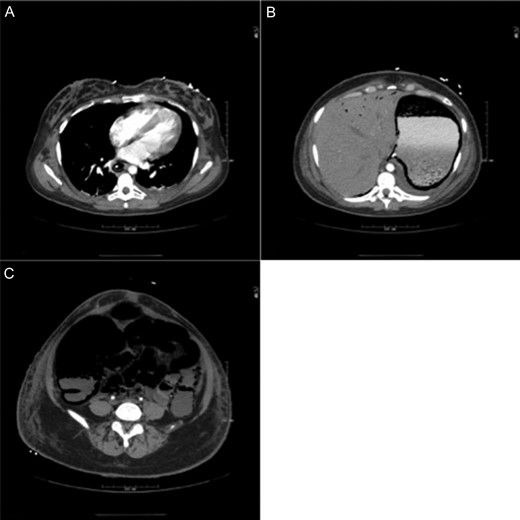
CT showing extensive pneumatosis involving the esophagus (A), the stomach (B) and the small bowel and colon (C). Hepatic portal venous gas is notable in (B).
After 48 h, the patient returned to the OR and the entire colon was frankly necrotic (Fig. 4) in addition to the terminal ileum. We proceeded with a subtotal colectomy and small bowel resection, leaving ~200 cm of jejunum and ileum. For end-ileostomy maturation, burn was first excised from the ileostomy site on the abdominal wall, and the site was allografted (150 cm2). This allowed ileostomy maturation in the standard fashion (Fig. 5). The abdominal fascia was then closed.

At the time of re-exploration, the colon from the ileocecal valve to rectosigmoid junction was frankly necrotic in addition to a 10 cm segment of small bowel near the prior resection. Orientation: left side of image is caudal, right side of image is cranial.
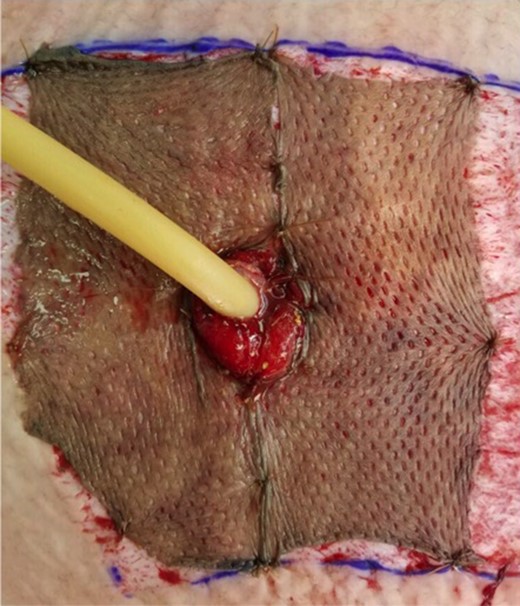
The end-ileostomy site was covered with human cadaver allograft prior to maturing the ileostomy in the standard fashion. A malecot drain is seen in the image.
After a post-operative ileus, enteral feeds were restarted on PBD 15 (post-bowel resection Day 11). A CT on PBD 19 for infectious work-up demonstrated resolution of pneumatosis and HPVG (Fig. 6). Excision of the burn wounds began on PBD 4 and was complete on PBD 50. The patient was discharged 2 months after burn injury. At the time of discharge, she had a functioning ileostomy and was tolerating an oral diet with appropriate nutritional parameters. She continues to recover well after her burn surgeries.

CT scan obtained on post-burn Day 19 demonstrating resolution of pneumatosis and hepatic portal venous gas.
DISCUSSION
GI complications occur in 1 in 20 severely burned patients with a mortality of 45% [2]. In burn patients IE has an incidence of 0.5% when clinically diagnosed, however, postmortem studies suggest up to 50% of burn patients have some degree of ischemic bowel injury [2]. Burn patients with massive intestinal infarction have a mortality >75% [3]. Non-occlusive mesenteric ischemia is the most frequent cause of GI infarction in burn patients as compared to the general population, where 80% of cases are the result of occlusive mesenteric ischemia [4].
Burn patients are at risk for ischemic bowel due to their massive fluid shifts, changes in cardiac output and decreased regional organ perfusion as a consequence of their decreased intravascular volume [3]. This emphasizes the importance of fluid resuscitation in the immediate post-burn period. However, large volume resuscitation may lead to bowel edema, ascites and intraabdominal hypertension which likely reduces venous outflow [5]. Additionally, early enteral nutrition has been implicated as playing a role in the development of bowel ischemia after severe burn injury [6]. However, early enteral feeding may be of benefit and there is no survival difference based on the timing or rate of initial tube feeding in burn patients [3].
In critically ill patients, the utility of the physical exam is unreliable. Worsening abdominal distention, peritoneal signs, or hematochezia should prompt radiographic evaluation. Huzar et al. identified PI or HPVG in 92% of patients with worsening clinical signs; intestinal ischemia was found in 93% of patients with PI. PI can be associated with bowel ischemia and poor outcomes [3, 7], however, its true incidence in the burn population is unknown [8]. The largest series to date reported a 1.3% incidence of PI with a median time from date of injury to diagnosis of PI of 10 days [3]. No patient developed PI earlier than 7 days after injury. Similar results have been reported by others [4]. In the series by Huzar et al. [3], survivors had smaller median TBSAs compared to non-survivors (27 vs 52%).
The development of a metabolic acidosis and increased serum lactate levels may also have a role as early markers of bowel ischemia [9]. Mortality and the risk of ischemic bowel are greater among patients with higher lactate levels and greater base deficits prior to the diagnosis of PI [3, 10]. In this case, new onset acidosis after successful burn shock resuscitation coupled with the extensive pneumatosis within 48 h of admission prompted emergent surgical intervention.
Overall, the authors believe there should be a low threshold for abdominal exploration in severely thermally injured patients with both radiographic evidence of PI and clinical decompensation. Tube feed intolerance, abdominal distension, worsening lactic acidosis or base deficit, and PI or HPVG are important factors to consider. Prompt diagnosis and successful management of the underlying condition ultimately contributed to this patient’s survival.
ACKNOWLEDGEMENTS
We thank the patient for allowing us to participate in her care and her consent to publish her case for the advancement of research and education.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- ischemia
- gastrointestinal tract vascular insufficiency
- acidosis, lactic
- body surface area
- burns
- infarction
- operating room
- peritonitis
- pneumatosis cystoides intestinalis
- surgical procedures, operative
- abdomen
- diagnosis
- small-intestine resection
- colon resection, partial
- thermal injury
- abdominal swelling
- intestinal wall



