-
PDF
- Split View
-
Views
-
Cite
Cite
Aniruddha A Sheth, Vinh Ngo, Mark Lam, Traumatic cerebrospinal fluid oculorrhea managed with an external ventricular drain, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy215, https://doi.org/10.1093/jscr/rjy215
Close - Share Icon Share
Abstract
Cerebrospinal fluid (CSF) leaks following head injuries are rare complications with significant morbidity and mortality if left untreated. CSF oculorrhea secondary to a cranio-orbital fistula is a rare presentation of this complication. Standard treatment for a CSF leak involves management of intracranial pressure, CSF diversion and surgical repair of any dural defect. Lumbar drains have commonly been inserted to aid in diverting CSF. We describe a case of a 16-year-old male who presented with an open comminuted depressed skull fracture and CSF oculorrhea. Following a bifrontal decompressive craniectomy, he was successfully treated with CSF diversion following a conservative trial using an external ventricular drain. The use of an external ventricular drain for this purpose has not been described in the literature to date. We report this case as a method of demonstrating the use of an external ventricular drain to adequately divert CSF.
INTRODUCTION
Cerebrospinal fluid (CSF) leaks following head injuries are a rare but significant complication. Young males are at the highest risk of developing a post-traumatic CSF fistula. Those with anterior cranial fossa fractures are the group at highest risk of a CSF fistula due to a minimal dural investment with only arachnoid mater covering at limited points on the calvarium and a thinner skull [1]. Cranio-orbital CSF fistulas are a rare complication of anterior cranial fossa injuries with a building number of cases in the literature recently [2, 3]. The cases have been managed with conservative and surgical therapy. Conservative therapy includes preventing intracranial hypertension and CSF diversionary procedures such as lumbar or external ventricular drains [1, 2]. We describe a case of a patient managed with an external ventricular drain as a CSF diversionary procedure which has not been described in the literature to date.
CASE REPORT
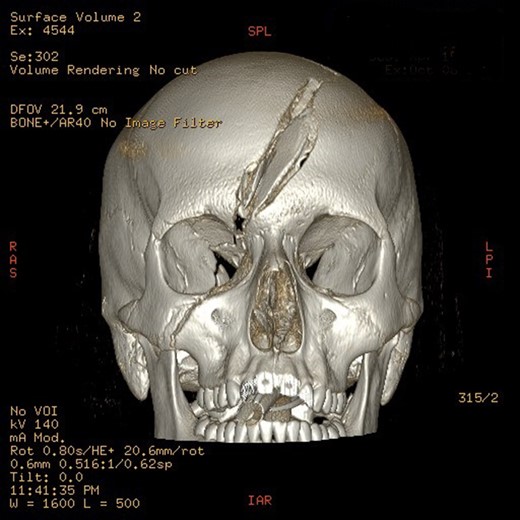
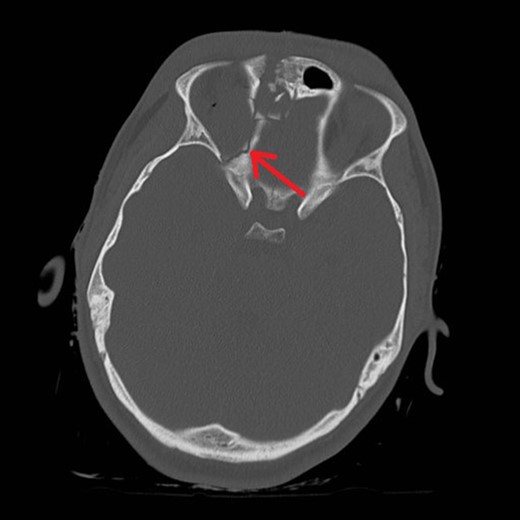
Mr AB is a 16-year-old male multi-trauma patient secondary to a high speed motor vehicle accident. His injuries included a frontal open comminuted depressed skull fracture with a fragment displaced and abutting the superior sagittal sinus (Fig. 1). The fracture line involved the right medial orbital wall extending through the ethmoid air cells and roof of the right sphenoid sinus (Fig. 2). Other cranial injuries included a fracture through the right side of the greater wing of the sphenoid bone, frontal intraparenchymal contusions and a traumatic subarachnoid/subdural haematoma. He had a laceration extending across the left side of his forehead to the medial canthus. His extracranial injuries included proptosis of his right eye, a closed unstable pelvic fracture with involvement of the left superior gluteal artery and a subcapsular liver haematoma.
His GCS at the scene was 6 (E1V2M3) where he was intubated by the paramedical officers and admitted to the State Major Trauma Unit and managed in the intensive care unit. The decision was made to medically manage his intracranial pressures for 7 days prior to surgically treating his skull fractures with intracranial pressure monitoring. He also underwent a right lateral canthotomy, approximation of his forehead laceration and application of a pelvic binder.
He was noted to have clear low flow discharge from his right medial canthus on Day 3 of his stay with a beta-trace protein level of 11.0 mg/l confirming a CSF leak. The decision was made to continue with non-surgical intracranial pressure management till Day 7 of his admission. During the period of non-operative management, his intracranial pressures were labile requiring maximal levels of sedation, neuromuscular paralysis and osmotic therapy with hypertonic saline. It was not possible to maintain a lateral decubitus position to insert a lumbar drain due to the presence of his pelvic fracture and labile intracranial pressure.
On Day 7 of his admission, a frontal craniotomy, removal of fragments, ligation of the superior sagittal sinus, repair of dural lacerations, right frontal external ventricular drain insertion, right frontal intracranial pressure monitor insertion and repair of frontal bone fractures were performed. It was not possible to primarily close the dura due to the extent of the dural lacerations and oedematous brain. Duraform was used as an overlay with a pericranial graft. This was an uncomplicated procedure. By the first 10 post-operative hours, he had developed medically refractory raised intracranial pressures. He was taken back to theatre for a bifrontal decompression at this stage. The external ventricular drain was left in situ due to the presence of the CSF oculorrhea.
Following his bifrontal decompression, he had no further episodes of intracranial hypertension. His CSF oculorrhea ceased on post-operative Day 6 following continued CSF diversion. The EVD output was maintained at 5–10 ml/h with the height 3 cm above the level of the tragus. The EVD was removed on post-operative Day 10 after being clamped for 24 h. There was no further CSF oculorrhea.
The patient has subsequently undergone an autologous cranioplasty. There has been no note of meningitis or pneumocephalus 2 months following his admission.
DISCUSSION
CSF oculorrhoea is formed due to a persistent fistula between the cranium and orbit. There are four key anatomical locations, that when damaged, are prone to causing CSF oculorrhea. These are the frontal sinuses, the cribriform plate and ethmoid roof, sphenoid sinus and petrous bone [3]. The route of CSF leak is commonly associated with a dural tear, the fractured bone and through the conjunctiva [3, 4]. Pease et al. [3] described damage to the cribriform plate and medial orbital wall allowing CSF drainage via the ethmoidal air cells. True oculorrhea requires breach of the conjunctiva and meninges [3]. He underwent a lateral canthotomy which involves dividing the conjunctiva as part of the procedure [5]. Our patient had a clear dural laceration due to the comminuted fracture demonstrated intraoperatively. His medial orbital wall and ethmoidal fracture suggested that this was the likely route of CSF drainage.
CSF oculorrhea most commonly presents with visible trauma to the orbit or face. It can also present with epiphora, orbital cyst formation, ocular involvement with loss of movement or pupillary reflexes [3]. Diagnosis is commonly established with laboratory analysis of the beta-trace protein level in the fluid [6]. Conservative management involves reducing intracranial pressure with bed rest, head elevation, avoiding hypertension and reducing intra-abdominal/intrathoracic pressure [1]. If this fails, a surgical approach can be taken to primarily repair the dural defect. A decompressive craniectomy has not been described as an option in the treatment of CSF fistulae [7, 8].
CSF diversion options include intermittent or continuous lumbar or ventricular drainage for up to 10 days [1]. The recommended rate of CSF drainage is 5–10 ml/h [1]. The patient in this case underwent adequate CSF diversion following his trial of conservative treatment. He demonstrated a leaking CSF fistula following his decompressive craniectomy with normal intracranial pressures. We have demonstrated the use of an external ventricular drain draining at the same rate as a lumbar drain in the treatment of this fistula. We believe that this demonstrates a novel method of CSF diversion for the management of a traumatic cranio-orbital fistula.
CONFLICTS OF INTEREST STATEMENT
None declared.



