-
PDF
- Split View
-
Views
-
Cite
Cite
Marta R P Costa, Ana S B Matos, João R Almeida, Fernando J Oliveira, Primary gastric volvulus: a report of two cases, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy227, https://doi.org/10.1093/jscr/rjy227
Close - Share Icon Share
Abstract
Gastric volvulus is an uncommon cause of gastric obstruction. It can be classified as primary when no underlying condition is identified as the cause for the rotation. An acute presentation includes typical symptoms and is frequently detected by imaging studies. Chronic cases present with intermittent vague symptoms and imaging studies may be normal during the symptomatic interval. The lack of specific symptoms and signs delays the diagnosis of chronic volvulus. However, appropriate treatment demands prompt diagnosis. We report two cases of primary gastric volvulus, with chronic or subacute symptoms and normal imaging studies during the asymptomatic periods. Both were treated surgically and had an uneventful follow-up.
INTRODUCTION
Gastric volvulus (GV) is a rare clinical condition, defined as the pathological rotation of the stomach by more than 180° [1–3].
Clinical presentation may vary from occasional non-specific symptoms to life-threatening situations [4]. Complete volvulus may result in a closed loop obstruction with strangulation. Mortality rates may be as high as 30–50%, in result of delayed recognition and treatment [2–6]. It is critical to secure an early diagnosis in order to allow for prompt treatment. The optimal treatment strategy for patients with GV has not been established [7].
We report two cases of primary GV, presenting with chronic/subacute symptoms, which underwent a successful surgical treatment.
CASE REPORT 1
An 80-year-old woman presented to the emergency department with a 12-h history of epigastric pain and vomiting. Physical examination revealed a slight tenderness to palpation of the epigastrium.
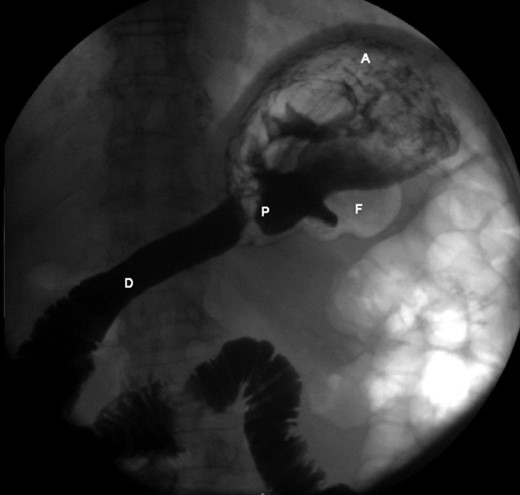
The patient’s leucocyte count and serum amylase presented mildly elevated. Chest radiograph revealed an elevated left hemi-diaphragm. Abdominal radiographs demonstrated a spherical stomach, presupposing an upward position of the pylorus (Fig. 1).

Abdominal radiograph, demonstrating a spherical stomach, presupposing an upward position of the pylorus.
A nasogastric tube was placed, draining immediately 2000 ml of gastric fluid. The patient had a complete relief of her symptoms and was admitted to the surgical ward for further study and clinical surveillance.
An upper endoscopy was performed, revealing a severe esophagitis with a distortion of the gastric anatomy. A great amount of stasis fluid and multiple ulcerations of the gastric fundus were present. An upper gastrointestinal series was also performed, revealing an inverted stomach, with the atrum being positioned superiorly to the fundus, with an abnormal position of the pylorus (Fig. 2).
Upper gastrointestinal series, revealing an inverted stomach, with the atrum being positioned superiorly to the fundus and a stretched duodenal arch, with an abnormal position of the pylorus.
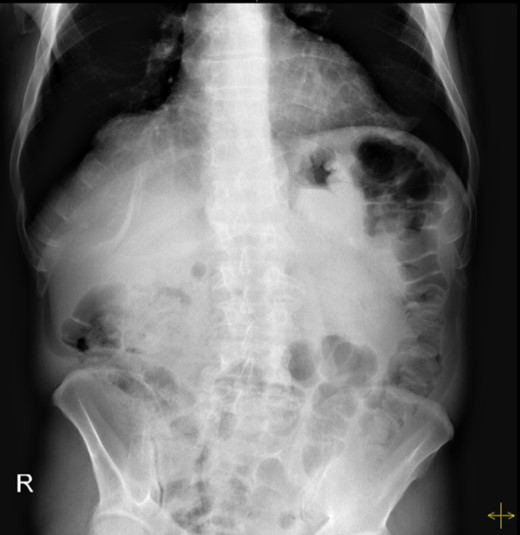
The patient was submitted to exploratory laparotomy, during which a mesenteroaxial GV was found, showing great laxity of the peritoneal ligaments and a bulky stomach (Fig. 3). The surgeons decided to perform a partial gastrectomy, from which the patient recovered uneventfully. She was discharged on the ninth post-operative day and presented no complaints 1 year after the surgery.
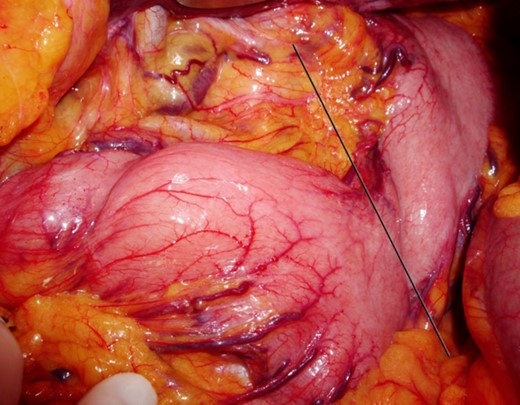
Findings during exploratory laparotomy, showing great laxity of the peritoneal ligaments and a bulky stomach.
CASE REPORT 2
A 60-year-old man presented with multiple episodes of upper abdominal pain, associated with retching and vomiting. These events usually happened in the morning, before breakfast, and resolved spontaneously after vomiting. Physical examination noted only mild tenderness on upper abdominal examination.
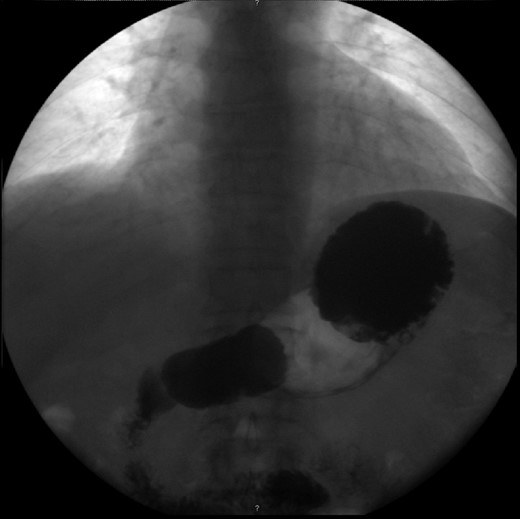
Haematological and biochemical profiling were performed, as well as plain abdominal radiographs (Fig. 4) and abdominal ultrasound, all showing no relevant changes. The upper endoscopy revealed a mild esophagitis. An upper gastrointestinal series was later executed, revealing the presence of an organoaxial volvulus (Fig. 5).
Abdominal radiograph performed during a symptomatic interval, showing no relevant changes.
Upper gastrointestinal series, revealing an organoaxial torsion of the stomach.
The patient was submitted to exploratory laparoscopy, which confirmed the diagnosis and revealed a large and bulky stomach, with signs of diminished vascular supply. Therefore, the surgeons decided to perform a partial gastrectomy, from which the patient recovered uneventfully. Pathologic examination confirmed the diagnosis and showed ischaemia of the gastric mucosa. He was discharged on the sixth post-operative day and presented no complaints 2 years after the surgery.
DISCUSSION
GV is defined as an abnormal rotation of the stomach, which can create a closed-loop obstruction, resulting in strangulation [3, 8]. Approximately 80% of GV cases occur in adults [5, 6, 8]. The exact incidence of GV is unknown and patients with a chronic presentation may never be diagnosed [7].
The volvulus can be classified as organoaxial, where the stomach rotates around an axis that connects the gastroesophageal junction and the pylorus; mesenteroaxial, where the rotation occurs around an axis that bisects both the lesser and greater curve; or mixed. Strangulation is less likely to occur in mesenteroaxial volvulus, where spontaneous detorsions with recurrent acute episodes may occur [9].
Primary GV (25–30%) has been associated with the absence or laxity of the gastrocolic or gastrosplenic ligaments [2, 4, 5]. Secondary GV (70–75%) is always associated with an underlying condition such as paraesophageal and diaphragmatic hernias, connective tissue disorders, adhesions and anterior abdominal wall defects [3, 5, 10]. Both of the cases we reported can be classified as primary.
The clinical presentation of GV depends on the degree of rotation and the rapidity of onset [1, 6, 10]. Acute GV usually presents with abdominal or chest pain, severe vomiting and epigastric distension. Borchardt triad (pain, retching and inability to pass a nasogastric tube) occurs in up to 70% of cases [4, 5]. Even with appropriate treatment, mortality of acute volvulus varies from 30 to 50% [10]. Chronic volvulus presents with broad-spectrum symptoms, which may include non-bilious vomiting, epigastric pain or distension, early satiety, retching and gastro-oesophageal reflux [4]. Both cases here described presented as chronic GV, with intermittent symptoms.
The diagnosis is frequently made by an abdominal radiograph and an upper gastrointestinal series, which is considered the diagnostic tool of choice, although the results may be normal during the asymptomatic period [4]. CT scan provides more accurate diagnosis with specific details of the anatomical abnormalities [2, 7]. On endoscopy, distortion of gastric anatomy with difficulty intubating the stomach or the pylorus is highly suggestive. Progressive ischaemic ulceration, or mucosal fissuring suggests late stage disease with strangulation [2].
Acute GV is an abdominal emergency and early surgery is mandatory. Delayed diagnosis may result in strangulation, ischaemia and necrosis with perforation, leading to shock [3, 10]. As for treatment of chronic GV, while surgery is the preferred treatment for most authors, others claim that it can be managed conservatively with prokinetic agents and anti-secretory therapy. It is important for clinicians to take patients age, comorbidity, physical performance, life expectancy and willingness into consideration [7].
Definitive treatment includes gastric decompression, reduction of the volvulus, repair of the predisposing structural defects and fixation of the stomach to prevent recurrence. Non-viable or gangrenous areas may demand subtotal or total gastrectomy. Our surgical team decided in both cases for a partial gastrectomy, due to intraoperative findings and both patients recovered well, with no recurrence of symptoms.
CONCLUSION
GV is an unusual entity, often not recognized at an early stage, which can become a surgical emergency. Primary GV is not associated to any underlying condition and presents more frequently with intermittent symptoms. Non-specific and misleading symptoms and signs may delay the diagnosis. Imaging, performed in the asymptomatic period may be non-diagnostic. Surgical treatment should be performed according to aetiology and to patient’s characteristics.
CONFLICT OF INTEREST STATEMENT
None declared.



