-
PDF
- Split View
-
Views
-
Cite
Cite
Jason Bowman, Bryan Curnutte, Kyle Andrews, Jacob Stirton, Nabil Ebraheim, Abdoul Azim Mustapha, Lateral intermuscular septum as cause of radial nerve compression: case report and review of the literature, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy226, https://doi.org/10.1093/jscr/rjy226
Close - Share Icon Share
Abstract
Multiple sites of compression of the radial nerve have been described, some more commonly than others. In this case report we describe a case of radial nerve compression at the lateral intermuscular septum in a patient with a history of open reduction and internal fixation of a mid-shaft humerus fracture 10 years prior. To our knowledge, only one previous case of chronic radial nerve compression by the lateral intermuscular septum associated with a humeral shaft fracture has been described. Our patient’s clinical presentation with specific electrodiagnostic abnormalities, operative findings and post-operative symptom relief point towards the rare diagnosis of compression of the radial nerve at the level of the lateral intermuscular septum as the cause of his symptoms.
INTRODUCTION
Numerous sites of radial nerve compression have been described along its course from the posterior cord of the brachial plexus to its terminal branches, the posterior interosseous nerve (PIN) and the superficial branch of the radial nerve (SRN). Common compression sites of the radial nerve include the spiral groove of the humerus, particularly following a mid-shaft humerus fracture, distal to the elbow in the radial tunnel and proximal to the wrist between the brachioradialis and extensor carpi radialis longus [1, 2].
Less common sites of radial nerve compression occur in the axilla in patients with an accessory subscapularis-teres-latissimus muscle, in the triangular space, within the lateral head of the triceps, and where the radial nerve penetrates the lateral intermuscular septum. Few cases have been reported of these less common sites of radial nerve compression [3, 4], but clinicians must be familiar with these sites to ensure a timely and accurate diagnosis because a delay in treatment is often associated with a poor recovery of nerve function [1, 5].
Here we describe a case of radial nerve compression at the lateral intermuscular septum in a patient with a history of open reduction and internal fixation of a mid-shaft humerus fracture 10 years prior.
CASE REPORT
ML is a 52-year-old male who presents to our clinic complaining of severe left anterolateral arm pain after being involved in a motor vehicle accident 10 years prior to presentation. At that time, he had suffered a left mid-shaft humerus fracture treated with open reduction and internal fixation, as well as a traumatic brain injury and multiple other injuries to the right lower extremity resulting in the below-knee amputation. For the last several years he has had severe pain in the anterolateral aspect of the left arm, but denies any weakness or parasthesias. On physical examination, he demonstrates localized tenderness to palpation along the anterolateral aspect of the mid-humerus ~8–10 cm proximal to the lateral epicondyle. The patient had full motor function, though somewhat limited by pain, and sensation was intact to light touch throughout the radial nerve distribution. Plain films (Fig. 1) and CT-imaging (Fig. 2) show a healed fracture with acceptable alignment and hardware in good position. The patient elected to undergo lidocaine injection at the site of maximal tenderness, which gave excellent, albeit temporary pain relief, for about a week. Electrodiagnostic studies obtained at that time revealed chronic radial nerve neuropathy above the spiral groove.
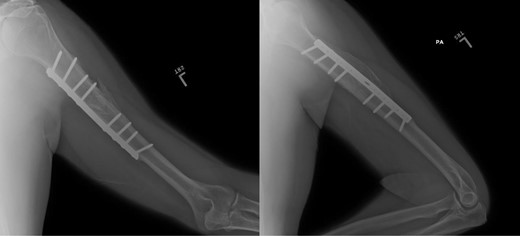
Plain films, AP/lateral showing appropriate alignment of fracture.
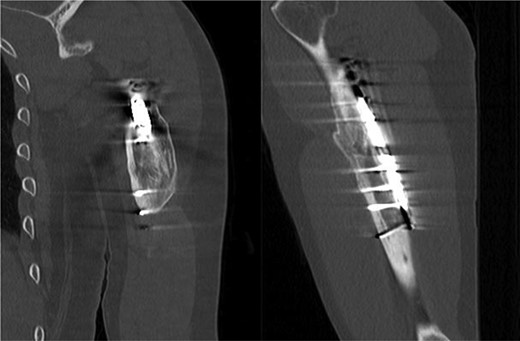
CT, coronal/sagittal showing a healed mid-shaft humerus fracture.
Surgical risks, benefits and alternatives were discussed and the patient elected to proceed with left radial nerve neurolysis and decompression. An anterolateral approach to the humerus was utilized with the incision centered over the point of maximal tenderness. Dissection was carried down to the biceps, which was retracted medially. The fascia over the brachialis and brachioradialis was then incised and the plane between these two muscles was bluntly developed with finger dissection. The radial nerve was then identified in the distal portion of our field and traced proximally to the lateral intermuscular septum. Significant compression of the radial nerve was noted proximally as it pierced the lateral intermuscular septum. No abnormal callous or fibrous tissue was appreciated, nor other sites of compression or adhesions were noted. The compressive septum was released while protecting the nerve and the wound was irrigated and closed. In the post-operative care unit the patient said that he could immediately feel that the deep pain that had been there for years was gone. At the 10-day post-operative visit, the patient reported that his preoperative pain had completely resolved with continued full motor and sensory function in the radial nerve distribution, therefore, a repeat electrodiagnostic study was not performed. At most recent follow-up, 4 months following surgery, the patient continues to report 0 out of 10 pain and states subjective improvement in function secondary to pain relief.
DISCUSSION
There are many potential sites of compression of the radial nerve along its course from the posterior cord of the brachial plexus to its terminal branches: the PIN and the SRN. The radial nerve courses along the posterior wall of the axilla, exits posteriorly through the triangular interval, running between the long head of the triceps and the humerus. It then courses distally in the spiral groove between the medial and lateral heads of the triceps before piercing the lateral intermuscular septum and entering the anterior compartment of the arm. At the level of the elbow, the radial nerve branches into the SRN and the PIN. The PIN dives under the supinator muscle at the arcade of Frohse before winding around the radial neck to the posterior compartment of the forearm, coursing toward the wrist deep to the brachioradialis and terminating in the base of the fourth extensor compartment at the dorsal wrist capsule.
The radial nerve proper can be compressed as it proceeds through the triangular space between the humerus and the long head of the triceps, and through the lateral head of the triceps [4]. Another potential, but uncommon site of compression is at the lateral intermuscular septum where the radial nerve passes from the posterior to the anterior compartment of the arm [3, 4, 6].
Two clinically distinct and commonly described entities of PIN compression are radial tunnel and PIN syndrome. The most common presenting symptom in radial tunnel syndrome is pain with the point of maximal tenderness representative of the site of compression. Electrodiagnostic studies are typically normal as there is no motor denervation [4]. In contrast, PIN syndrome usually presents as pain and weakness in the nerve distribution with positive electrodiagnostic findings [4]. Both of these entities involve the same potential points of compression: fibrous bands anterior to the radiocapitellar joint, the leash of Henry, the medial edge of the extensor carpi radialis brevis (ECRB), the arcade of Frohse and the distal edge of the supinator.
Lastly, the SRN can be compressed proximal to the wrist between the brachioradialis and the extensor carpi radialis longus [2] in a condition known as Wartenberg’s syndrome.
Radial nerve palsy occurs in 2–17% of cases with humeral shaft fractures [1]. Radial nerve palsy following mid-shaft humerus fractures may occur at the same time as the injury or present months to years following the injury [1, 3, 7, 8]. Neuropraxia accounts for nearly 90% of radial nerve palsies associated with humeral shaft fractures and are typically treated by observation for 3–6 months with exploration reserved for those cases that do not recover [1, 9]. Early exploration is recommended in open fractures, closed fractures where adequate closed reduction cannot be obtained, polytrauma patients and fractures with vascular injury [9]. Cases of chronic or delayed radial nerve palsy due to hematoma, axillary crutches or entrapment in fracture callus have been described as well [7, 8].
The lateral intermuscular septum separates the anterior and posterior compartments of the arm and extends from the crest of the greater tuberosity of the humerus to the lateral epicondyle where it becomes confluent with the annular ligament encircling the radial head [10]. The radial nerve travels through a defect in the lateral intermuscular septum with a mean diameter of 1 cm [10]. Cases of radial nerve entrapment in the fibrous canal proximal to the lateral intermuscular septum have previously been described post-traumatically and in patients with no prior history of trauma [3, 6]. These patients presented with lateral arm pain, local tenderness and a positive Tinel’s sign at the mid-third of the upper arm [6]. However, in our search of the literature, only one previous case of chronic radial nerve compression by the lateral intermuscular septum associated with a humeral shaft fracture was found [4]. This patient’s clinical presentation with specific electrodiagnostic abnormalities, operative findings and post-operative symptom relief point towards compression of the radial nerve at the level of the lateral intermuscular septum as the cause of his symptoms.
CONCLUSION
There are many possible sites of radial nerve compression along its course through the upper extremity. Surgical decompression can result in excellent pain relief and functional improvement when non-operative measures fail. While very uncommon, the lateral intermuscular septum is a possible site of nerve compression and should be considered in situations such as this.
CONFLICT OF INTEREST STATEMENT
None declared.



