-
PDF
- Split View
-
Views
-
Cite
Cite
Sima Sayyahmelli, Hakan Kina, Melih Ucer, M Shahriar Salamat, Mustafa K Baskaya, Frontal lobe intracerebral schwannoma mimicking metastatic lesion in a patient with papillary thyroid carcinoma, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy212, https://doi.org/10.1093/jscr/rjy212
Close - Share Icon Share
Abstract
Intracerebral schwannomas are quite rare. Due to their rarity and lack of pathognomonic imaging features, intracerebral schwannoma may be overlooked in the initial differential diagnosis of an intra-axial mass with heterogeneous ring enhancement, such as a high-grade glioma, metastasis or lymphoma. Here, we present a 21-year-old woman with prior diagnosis of papillary thyroid carcinoma and recent history of seizures who had a heterogeneously ring-enhancing left frontal lobe mass. Our presumptive diagnosis was a metastatic tumor since she had a history of thyroid cancer. Because of uncertainty in preoperative differential diagnosis, the decision was made to proceed with excisional biopsy of the tumor via craniotomy. She underwent uneventful gross total resection of the tumor that histopathology revealed as an intracerebral schwannoma.
INTRODUCTION
Intracerebral occurrences of schwannomas are uncommon, with the first known report in 1966 by Gibson et al. [1]. Since then, over 65 additional cases of intracerebral schwannomas have been described [2, 8]. These lesions are generally solitary. An association with neurofibromatosis was described in some reports [6, 9]. Prospective imaging diagnosis is challenging due to a lack of pathognomonic features [2]. Although common neuroradiological characteristics of intracerebral schwannoma are thought to be calcifications, cystic formations and peritumoral edema, these findings are not the rule [8]. The treatment of choice is complete surgical excision, which is associated with a good long-term outcome [6]. In this report, we review the clinical features and histopathology of an intracerebral schwannoma involving the left frontal lobe of a 21-year-old woman with the history of resected papillary thyroid carcinoma.
CASE REPORT
A 21-year-old woman, two years status post resection of a papillary thyroid carcinoma, presented to the emergency department with recent onset seizures. She had suffered from secondarily generalized tonic-clonic seizures that lasted for 1–2 min with a short postictal period. There was no diagnosis of neurofibromatosis and no other known genetic disorder in this patient or her family. On admission, the examination was unremarkable. She did not have any stigmata of neurofibromatosis. Neurological examination did not reveal any focal signs or deficits. Computerized tomography (CT) scans revealed a 2.6 × 2.4 cm2 heterogeneous left frontal lobe mass, with a hyperdense peripheral rim and surrounding vasogenic edema.
Magnetic resonance imaging (MRI) of the brain demonstrated an intra-axial left frontal lobe mass that was hypointense with an isointense rim on T1 (Fig. 1), mixed isointense and hyperintense on T2 (Fig. 1), with extensive surrounding vasogenic edema. The mass revealed a heterogeneous ring enhancement with a central area of non-enhancement (Fig. 1) and restricted diffusion within the wall of the mass. There was no evidence of hemorrhage or calcification observed using susceptibility-weighted MRI images or with CT imaging (Fig. 1). Although our presumptive diagnosis was a metastatic thyroid cancer, initial diagnosis also included primary high-grade glioma and lymphoma.
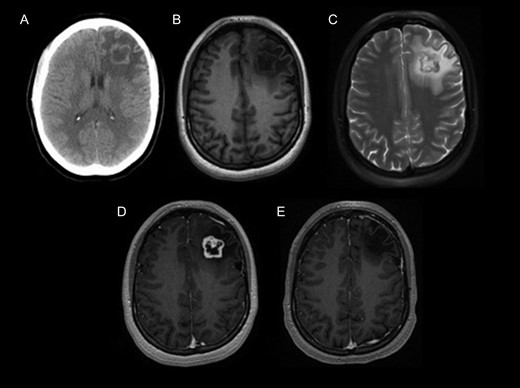
MRI tomography. (A) Non-contrast computed tomography shows heterogeneous left frontal lobe mass with a hyperdense peripheral rim and surrounding vasogenic edema without calcification. Pre-contrast (B) and post-contrast (C) T1-weighted MRI images, and T2-weighted MRI (D), show an intra-axial heterogeneously enhancing left frontal lobe mass with surrounding vasogenic edema. (E) 5-Year postoperative T1-weighted post-contrast MRI shows gross total resection of the tumor without recurrence.
A decision for microsurgical resection was made. The patient underwent a left frontal craniotomy. Gross total resection was achieved (Fig. 1). The intraoperative interpretation was a low-grade spindle cell neoplasm consistent with low-grade astrocytoma. The patient tolerated the surgery well, with an uneventful postoperative course. She was discharged home without any complications. A 6-year post-surgery follow-up did not reveal recurrence or neurologic deficit. The pathology from paraffin embedded tissue sections revealed a well-circumscribed spindle cell neoplasm, with a biphasic pattern of hypo and hyper-cellularity, surrounded by a thin rim of gliotic cerebral parenchyma. The spindle cells contained scant cytoplasm and elongated nuclei (Fig. 2). Focally a palisaded pattern was suggested. Abundant hyalinized blood vessels were also present. These were diagnostic features of a schwannoma with no anaplastic properties.
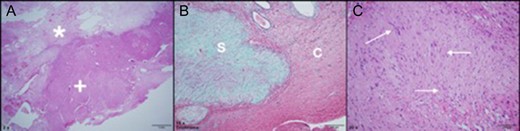
Tumor pathology (formalin fixed paraffin embedded). (A) Tumor at low magnification reveals a biphasic pattern of a loose collagenous central zone (*) and a compact peripheral zone (+), H&E stained, original magnification ×2. (B) Trichrome stain reveals a well-circumscribed collagen-rich schwannoma (S, green color) separated from the adjacent gliotic cerebral parenchyma (C), original magnification ×10. (C) At higher magnification, this H&E stained section reveals a palisaded pattern of neoplastic spindle cell nuclei (arrows), original magnification ×20.
DISCUSSION
Intracerebral schwannomas, without any apparent connection to cranial nerves, are exceedingly rare [8, 9]. Ectopic schwannomas account for <1% of surgically treated schwannomas of the central and peripheral nervous system [9]. In earlier reports, the majority of tumors were located in the temporal and frontal lobes, which are more prone to development of schwannoma-associated seizures [9]. Intracerebral schwannomas can resemble other more common intra-axial cystic neoplasms including high-grade gliomas [3].
Some reports indicate that men are found to be more often affected than women [6–8] while others report no gender bias [5]. Commonly, patients present with headache and seizures [7, 8]. These tumors generally occur either in the first two decades life, with a slow indolent course or in the elderly with a rapid course [6]. Seizures are regarded as the most common symptom [9].
The origin of intracerebral schwannomas is much debated in the literature [2]. Since Schwann cells are not indigenous to cerebral parenchyma, substantial speculation has been attached to their origin [6]. There are two main theories for their occurrence in the central nervous tissue. One is that they have a developmental origin related to native CNS cells, such as the mesenchymal pial cells or neural crest cells. Another theory attributes the presence of Schwann cells to the perivascular nerve plexuses of penetrating vessels [2, 4].
The MRI characteristics of intracerebral schwannomas are variable, with T1 isointensity and hypointensity and mixed T2 isointensity and hyperintensity. They reveal intense but often inhomogeneous contrast enhancement depending on calcification, or the presence of cystic and/or necrotic components [8]. Due to the rare intracerebral occurrence and lack of pathognomonic imaging features [6, 9], an intracerebral schwannoma may mimic metastasis, primary high-grade gliomas or lymphomas. Further, their radiological findings are difficult to differentiate from high-grade gliomas [6]. Several characteristic findings have been described, although significant variability exists. These lesions are often superficial or periventricular in location and may be enhanced homogenously or heterogeneously [2, 5]. The presence of a cyst has been the most consistent finding with these tumors [6].
In the present case, the lesion had heterogeneous ring enhancement with extensive peritumoral edema without either a cystic component or calcifications. This led us to consider a high-grade glioma, a lymphoma, or a metastatic tumor as the potential differential diagnosis. Care must be taken to include schwannomas in the differential diagnosis of solid brain lesions. Since schwannomas are benign, complete excision is the treatment of choice [6].
In summary, although MRI characteristics can help in the differential diagnosis of mass lesions, especially in patients with a high index of suspicion in proper clinical settings, a neurosurgeon should consider other possible diagnosis. Excisional biopsy remains crucial in such cases for definite diagnosis. We recommend maximal safe resection in intracerebral schwannomas.
CONFLICT OF INTEREST STATEMENT
We report no conflicts of interest.



