-
PDF
- Split View
-
Views
-
Cite
Cite
Ibrahim Albabtain, Hassan Arishi, Slava Albaghli, Jumanah Aljahani, Inflammatory fibroid polyps of the appendix: different presentation and literature review, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy200, https://doi.org/10.1093/jscr/rjy200
Close - Share Icon Share
Abstract
Inflammatory fibroid polyps (IFPs), or Vanek’s tumor, are rare benign mesenchymal lesions of the gastrointestinal tract (GIT). IFPs can be found throughout the GIT but most frequently in gastric antrum or ileum, with the appendix accounting for only <1% of all IFPs. The clinical presentation is usually vague yet depends on the location. We report a case of 50-year-old healthy male presented to the emergency department with a sub-acute complaint of non-specific abdominal pain, which was suspected to be appendicitis. Abdominal CT scan was done as well as colonoscopy and histopathology were scheduled. A week later, he presented in the clinic, still complaining of abdominal pain; thus, the decision was made to schedule him for laparoscopy with appendectomy. Finally, the post-operative course was unremarkable and the patient was discharged home. This is a rare case of IFPs originating in the appendix presenting as an atypical sub-acute appendicitis.
INTRODUCTION
Inflammatory fibroid polyps (IFPs), or Vanek’s tumor, are rare benign mesenchymal lesions of the gastrointestinal tract (GIT) [1]. It was first discovered in the stomach by Vanek in 1949 as sub-mucosal granuloma with eosinophilic infiltration [2]. Their pathogenesis and etiology is not fully understood [3].
IFPs can be found throughout the GIT but most frequently in the gastric antrum or ileum [4]. The appendix is a rare site (<1%) of all IFPs in the GIT, which as few case reports mention, presents as acute appendicitis [1, 5]. There are no definite signs and symptoms of IFP and the clinical picture depends on the location and size of the tutor [6]. Signs and symptoms include a dull aching abdominal pain, dyspepsia, intestinal obstruction and, rarely, acute appendicitis [4].
We present a case of IFP in the appendix with an unusual location and atypical presentation.
CASE REPORT
A 50-year-old male, with an unremarkable medical and surgical history, presented to the emergency department with a complaint of abdominal pain for 10 days. The pain started in right iliac fossa and was localized. It was associated with anorexia, nausea and fever 1 day prior to his presentation. The pain was aggravated by movement and relieved by simple analgesia. There was no history of vomiting, changes in bowel habits, or recent weight loss. On examination, the patient was looking healthy and was afebrile. The abdomen had minimal tenderness over the right iliac fossa with an absence of any other signs of acute appendicitis. Laboratory investigations were within normal limits. The Emergency Department physicians examined the patient initially and their impression was an atypical presentation of acute appendicitis. A computerized tomography (CT) scan of the abdomen was done and indicated a well-circumscribed hypodense lesion at the base of the appendix, measuring 2.6 × 2.4 cm2, with no calcification or abnormal enhancement. The distal part of the appendix was dilated, measuring 8 mm in diameter with no surrounding fat stranding or significantly enlarged lymph nodes (Fig. 1).
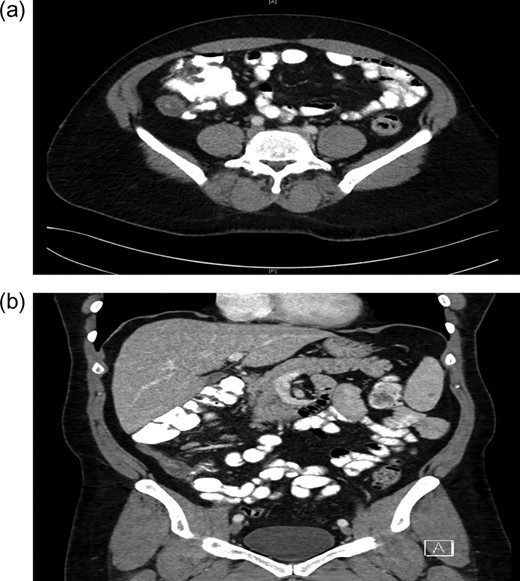
(a) Computed tomography of the axial view of abdomen showing mass in base of appendix. (b) Computed tomography of the coronal view of abdomen showing mass in base of appendix.
Upon the assessment of the surgical team, no sign of local peritonitis was appreciated and hence the decision was made to discharge the patient. A colonoscopy was scheduled after 3 days at the Outpatient Department to rule out other colonic masses. During colonoscopy, a 1 cm pedunculated polyp was found 20 cm from the anus. Snare polypectomy was done and histopathology results were indicative for tubular adenoma.
A week later, the patient was seen in the general surgery clinic, still complaining of abdominal pain. CT abdomen was repeated and showed the same findings. A decision was made to admit the patient with a possible diagnosis of an appendicular mucocele or less likely an appendicular carcinoid. A diagnostic laparoscopy with appendectomy and possible right hemi-colectomy was scheduled. Intra-operatively, the appendix was para-caecal and adherent to the caecum with a 3 cm cystic swelling of proximal appendix (Fig. 2). The caecum and ileum were normal and there were no peritoneal deposits. We managed to perform the appendectomy with an intact cystic mass.

The post-operative course was unremarkable and the patient was discharged on the third post-operative day.
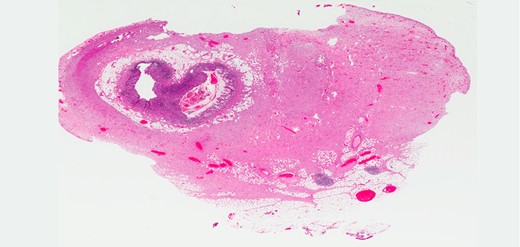
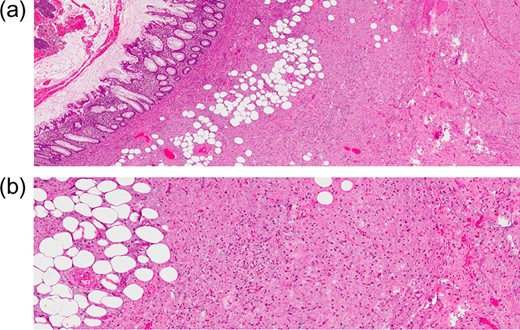
Histological examination showed an appendix measuring 7 cm in length and 0.8 cm in diameter with a cystic lesion at the base measuring 3.5 × 2.5 cm2. It had a grey homogenous cut surface invading the appendix wall while the mucosa was unremarkable. The mucosal lining showed elongated and dilated tubules with Goblet cell proliferation with no evidence of dysplasia. The sub-mucosa displayed an area of extensive edema, vascular congestion with focal hemorrhage and abundance of spindle cells, dispersed in a loose fibromyxoid stroma. The sub-mucosal background had copious eosinophils, lymphocytes and blood cells. There was no mitosis, acute inflammation, granuloma, ischemia or vasculitis (Figs 3–6). These findings are consistent with an appendicular IFP (Vanek’s tumor).
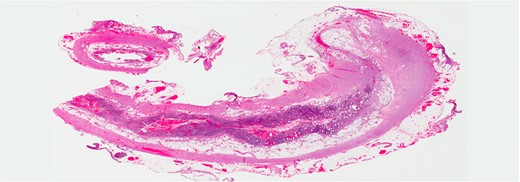
The tip and the middle part of the appendix with no specific pathology (H&E stain, low power).
The base of the appendix with the mass (H&E stain, low power).
(a) H&E stain of a lesion in the appendiceal wall with infiltrative nature (intermediate power). (b) H&E stain of abundant spindle cell, dispersed in loss fibromyxoid stroma, infiltrating the fat (high power).
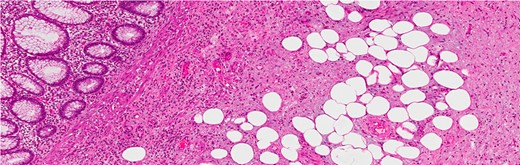
Infiltration into the sub-mucosa of the appendix (H&E stain, high power).
DISCUSSION
IFPs are rare, benign, idiopathic, pseudotumor, sub-mucosal neoplastic lesions originating in the GIT [3]. It was first described in the stomach by Vanek in 1949 as sub-mucosal granuloma with eosinophilic infiltration [2]. Grossly, they range from <1 to 20 cm with an average of 4.4 cm in diameter. Microscopically, these tumors are characterized by mononuclear, spindle cells, which are typically arranged in an onionskin-like fashion with sub-mucosal fibroblasts and vascular proliferation with eosinophilic infiltration and inflammatory process [4, 6]. Different names have been suggested for IFP in literature as eosinophilic granuloma, hemangiopericytoma, neurofibroma and polypoid fibroma. In 1953, the term IFP was first used by Helwig and Ranier for a gastric polyp, since then it gained acceptance for lesions throughout the GIT [4, 7, 8]. Genetic studies of IFP showed mutations in platelet derived growth factor alpha in some cases, which was previously thought to be reactive inflammatory lesions [4].
IFPs can be found anywhere in the GIT but most frequently in the stomach (70%), particularly in the antrum, followed by small intestines (20%), esophagus (2%), colorectal (5%) and appendix (<1%) [3, 4, 8, 9]. When found in the appendix, the size ranges from 2 to 8 cm [5, 10]. IFPs are diagnosed in both genders with a slight predominance in males and a peak incidence in the fifth and seventh decades [4].
They are usually asymptomatic and discovered incidentally during endoscopic procedures or a laparotomy. When symptomatic, the clinical presentation depends on the size and site of involvement. Gastric IFPs present with abdominal pain, whereas small intestinal lesions are often presented by intussusception, or obstruction. Vomiting, changes in bowel habits and lower gastrointestinal bleeding with anemia are less frequent symptoms [1, 3, 4, 6, 8, 9]. IFPs in the appendix have been reported in a few case reports with almost all of cases presenting as acute appendicitis [5, 10]. The presentation was acute within 48 h, whereas in our case, the presentation was sub-acute with non-specific abdominal pain (Table 1). The role of laboratory investigation and radiological imaging have minimal or no value in the diagnosis of IFP [4, 8, 9].
| Author . | Year . | Presenting symptoms . | Duration . | Procedure . | Size . |
|---|---|---|---|---|---|
| Kordzadeh A. | 2011 | Right iliac fossa pain, pyrexia, nausea | 2 days | Open appendicectomy | 2.6 × 2 cm2 |
| Sánchez-Cifuentes et al. | 2015 | Right lower quadrant pain | Acute? | Laparoscopic appendectomy | 5 cm |
| Chatelain et al. | 2008 | Abdominal pain and fever | 2 days | Laparoscopic appendectomy | 8 cm |
| Author . | Year . | Presenting symptoms . | Duration . | Procedure . | Size . |
|---|---|---|---|---|---|
| Kordzadeh A. | 2011 | Right iliac fossa pain, pyrexia, nausea | 2 days | Open appendicectomy | 2.6 × 2 cm2 |
| Sánchez-Cifuentes et al. | 2015 | Right lower quadrant pain | Acute? | Laparoscopic appendectomy | 5 cm |
| Chatelain et al. | 2008 | Abdominal pain and fever | 2 days | Laparoscopic appendectomy | 8 cm |
| Author . | Year . | Presenting symptoms . | Duration . | Procedure . | Size . |
|---|---|---|---|---|---|
| Kordzadeh A. | 2011 | Right iliac fossa pain, pyrexia, nausea | 2 days | Open appendicectomy | 2.6 × 2 cm2 |
| Sánchez-Cifuentes et al. | 2015 | Right lower quadrant pain | Acute? | Laparoscopic appendectomy | 5 cm |
| Chatelain et al. | 2008 | Abdominal pain and fever | 2 days | Laparoscopic appendectomy | 8 cm |
| Author . | Year . | Presenting symptoms . | Duration . | Procedure . | Size . |
|---|---|---|---|---|---|
| Kordzadeh A. | 2011 | Right iliac fossa pain, pyrexia, nausea | 2 days | Open appendicectomy | 2.6 × 2 cm2 |
| Sánchez-Cifuentes et al. | 2015 | Right lower quadrant pain | Acute? | Laparoscopic appendectomy | 5 cm |
| Chatelain et al. | 2008 | Abdominal pain and fever | 2 days | Laparoscopic appendectomy | 8 cm |
IFPs are benign and do not recur nor metastasize. The treatment is usually via endoscopy (endoscopic sub-mucosal dissection is required) or surgery (laparoscopic or open) depending on the location [4, 8]. Laparoscopic or open appendectomy is the treatment of choice for IFPs in the appendix [5, 10].
CONFLICT OF INTEREST STATEMENT
None declared.



