-
PDF
- Split View
-
Views
-
Cite
Cite
Michael Karanikas, Konstantinia Kofina, Ferdi Boz Ali, Vasileia Vamvakerou, Eleni Effraemidou, Nikolaos Lyratzopoulos, Alexandros Polychronidis, Primary greater omental torsion as a cause of acute abdomen—a rare case report, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy207, https://doi.org/10.1093/jscr/rjy207
Close - Share Icon Share
Abstract
Greater omental torsion is a rare entity that can cause acute abdominal pain, may mimick other abdominal pathologies, and is difficult to be diagnosed preoperatively. We present a case of a male patient with greater omental torsion mimicking the symptoms of acute appendicitis. A 31-year-old male patient presented with right scrotal pain, initially treated by the urologists, however, 24 h later, he presented right lower quadrant pain, with characteristics of acute appendicitis. After finding in ischemic inflammatory mass on McBurney incision, an exploratory laparotomy was performed, revealing torsion of the greater omentum. Torsion of the greater omentum can be a cause of acute abdomen and could be misdiagnosed with acute appendicitis. Preoperative diagnosis is not easy and resection of the affected tissue is the preferred treatment of choice.
INTRODUCTION
Torsion of the greater omentum is a rare, benign cause of acute abdominal pain, caused by twisting of the omentum around a pivotal point, usually in a clockwise direction [1]. Twisting causes compromised venous return, which leads to peritonitis and serosanguineous fluid accumulation in the peritoneal cavity, as well as arterial compromise, which induces ischemia and necrosis of the involved part [2]. Omental torsion can be primary or secondary [3], according to its correlation to pre-existing abdominal pathologies such as cysts, tumors, hernias or inflammation. It is rarely diagnosed preoperatively, as it presents no specific clinical findings, and can mimic other causes of abdominal pain [4].
Herein, we describe the case of a male patient who presented with clinical symptoms and laboratory findings of acute appendicitis, but was diagnosed with primary omental torsion intra-operatively.
CASE PRESENTATION
A 31-year-old male patient presented in the Emergency Department complaining of abdominal pain of rapid onset during the last 24 h, located mainly in the right scrotum, and mildly in the right iliac fossa. He mentioned mild nausea, but no vomiting or bowel dysfunction, and normal body temperature. His medical history included bilateral open inguinal hernia repair as an infant.
Clinical examination revealed tenderness in the right scrotum, with no palpable masses in the inguino-scrotal area; no specific signs for acute appendicitis were present. Laboratory blood examination showed an elevated white blood cell count (15.13 × 103/μL), as well as CRP levels (4.56 mg/dL). Ultrasound was negative for testicular torsion and fluid in the rectovesical pouch, but confirmed epididymitis, therefore, the patient was admitted to the Urology Department for the administration of antibiotics and analgesics. The following day the patient’s condition deteriorated, showing a further increase in CRP levels (17.52 mg/dl). Clinical examination revealed a positive McBurney’s sign and rebound tenderness. A second ultrasound was requested, whose findings were supportive of appendicitis, and the decision of surgical treatment was made.
Initially, under general anesthesia, a McBurney incision was performed, but an ischemic inflammatory mass and serosanguineous fluid were found; therefore, exploratory laparotomy through midline incision was considered necessary. The mass, identified as twisted omentum (Fig. 1), was dissected after ligation of the omental pedicle (Fig. 2). Additional appendectomy was performed to prevent any future diagnostic problems, while the rest of the abdominal cavity showed no underlying pathology or signs of adhesions.
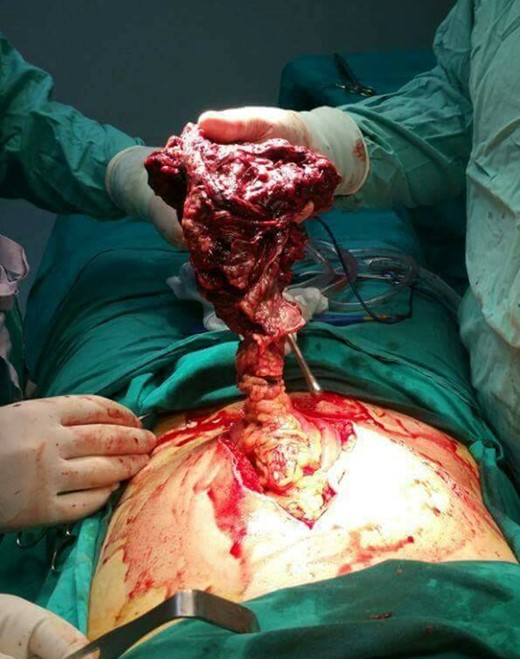
Torsion of the greater omentum. Intra-operative finding through exploratory laparotomy.

Post-operative recovery was uneventful and the patient was discharged 5 days after the surgery in good health condition. Histopathologic examination of the dissected omental mass showed extended hemorrhagic necrosis, accompanied by inflammatory infiltration, whereas the appendix (of 6.5 cm in length), presented serosal appendicitis secondary to the intra-abdominal inflammation.
DISCUSSION
Greater omental torsion presents an incidence of 0.0016–0.37% and is the cause of 1.1% of cases with abdominal pain [4]. It occurs due to twisting of a pedicle of the omentum along its long axis, which results to vascular compromise and, eventually, necrosis. The condition was first described by deMarcetti in 1858, while the first report of primary omental torsion came from Eitel in 1899 [5]. The condition mainly occurs in middle-aged adults, and is twice as common in men [2].
Pathogenesis of primary torsion remains unclear, though a variety of factors has been proposed. Formation around the right distal epiploic artery seems to be associated with the greater size and mobility of the omentum in this region. Predisposing factors mainly include anatomical variations such as tongue-like projections, bifid or accessory omentum and narrow omental pedicle. Obesity has also been widely accused of leading to torsion, due to excess fat deposit. Venous redundancy relative to the arterial blood supply is yet another factor, but also the veins, following a sinuous trail, allow the formation of a knob as a point of fixation [6].
Secondary torsion is related to intra-abdominal pathology, such as herniation, cysts, foci of inflammations, tumors and surgical wounds or scarring. Its frequency of appearance is significantly higher than that of primary torsion. In both primary and secondary, all causes of increased abdominal pressure could serve as precipitating factors. Those could be heavy meals, physical activity, sneezing, coughing, recent abdominal surgery or trauma, sudden changes in body position, increased peristalsis and even pregnancy [2]. Manual hernia reduction could also be considered as a factor in some cases [7].
Patients present with constant, non-radiating and gradually increasing, sudden pain [8]. Location of the pain depends on the torsion site and is usually localized in the right lower quadrant. Gastrointestinal symptoms, such as anorexia, nausea or vomiting are absent in over 50% of the patients, as intestinal peristalsis is not affected [4]. Leucocytosis and elevated body temperature could also occur, as well as a palpable mass, depending of the size of the segment involved. Therefore, differential diagnosis includes any other cause of acute abdomen.
Ultrasound typically shows a solid, non-compressible, hyperechoic mass found under the site of highest sensitivity. CT scan reveals a focal inflammatory mass of fatty density with streaks that form a whirling pattern, corresponding to fibrous bands or dilated veins [9]. The integrity of other abdominal organs is important as normal appendix, gallbladder and pelvic cavity can rule out other conditions and make omental torsion a likely diagnosis [10]. In our case, ultrasound did not show typical findings of greater omental torsion, whereas a CT scan was not performed, as it was not considered a routine test in cases of indicated acute appendicitis.
Accurate diagnosis using imaging techniques in an early stage can lead to conservative treatment. However, surgical intervention, open or laparoscopic, is the preferred choice for diagnosis and treatment; additional appendicectomy is widely described in literature, in order to avoid future diagnostic problems [10].
CONCLUSION
Greater omental torsion, although rare, can be the cause of abdominal pain and, therefore, should be included in the differential diagnose of pain in the right iliac fossa, which could mislead the surgeon to the diagnosis of acute appendicitis. As preoperative diagnosis is usually difficult, surgery is still considered the treatment of choice.
ACKNOWLEDGEMENTS
The authors certify that there are not any financial or non-financial competing interests.
CONFLICT OF INTEREST STATEMENT
None declared.



