-
PDF
- Split View
-
Views
-
Cite
Cite
Paul Chandler, Jonathan Harris, Danny Sherwinter, Adenomyomatous hyperplasia of distal common bile duct: a case report and review of the literature, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy204, https://doi.org/10.1093/jscr/rjy204
Close - Share Icon Share
Abstract
Adenomyomatous hyperplasia (AH) is commonly found in the gallbladder and is considered a tumor-like inflammatory lesion arising from Rokitansky-Aschoff sinus. It is extremely rare in the extrahepatic bile duct and only 15 cases have been reported to date. We describe a 63-year-old male patient who presented with cholangitis, underwent an extensive diagnostic workup, and ultimately had a Whipple procedure. Final pathology showed a 2.0 × 1.5 × 0.5 cm3 granular lesion in the distal common bile duct. There was prominent biliary epithelial proliferation with tubular–papillary architecture and minimal nuclear atypia in association with chronic inflammation, stroma reaction and smooth muscle proliferation. AH of the extrahepatic bile duct is a benign process but often requires a major operation to definitively diagnose.
INTRODUCTION
Adenomyomatous hyperplasia (AH) is commonly found in the gallbladder and is considered a tumor-like inflammatory lesion arising from Rokitansky-Aschoff sinus. It is extremely rare in the extrahepatic bile duct and only fifteen cases have been reported to date [1–9]. We describe a patient who presented with cholangitis, underwent an extensive diagnostic workup, and ultimately had a Whipple procedure for a distal common bile duct (CBD) lesion which was histopathologically diagnosed to be AH. We review the published reports of AH of the extrahepatic bile duct and discuss the diagnostic and clinical relevance to this case.
CASE REPORT
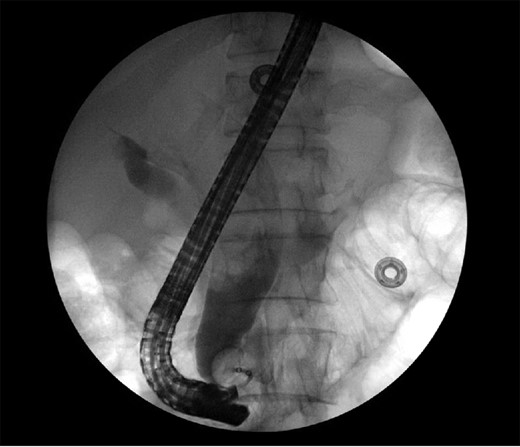
The patient is a 63-year-old Chinese male who presented with lethargy, 10-pound weight loss and painless jaundice for 1 week. Patient had a prior episode of jaundice of unclear etiology 2 years prior treated medically and had just emigrated from China 1 month prior to admission. Patient was febrile to 102.4°F, jaundiced with a total bilirubin of 18.5 mg/dL. Abdominal ultrasound showed intra and extrahepatic bile duct dilation, the distal CBD was dilated to 25 mm. Patient underwent endoscopic retrograde cholangiopancreatography (ERCP), which showed thick yellow mucus and no stones (Fig. 1). A sphincterotomy was performed and a pigtail stent placed. Computed tomography (CT), magnetic resonance imaging and magnetic resonance cholangiopancreaticogram failed to show a pancreatic head mass, distal CBD mass or stones causing obstruction (Fig. 2). Cold forceps biopsy of the papilla, endoscopic ultrasound with fine needle aspiration biopsy (FNAB) of pancreatic head, and CBD brushings were all nondiagnostic. CBD stents occluded two times in 2 weeks’ time secondary to thick mucus, requiring multiple ERCPs with stent exchanges (Fig. 3). After extensive multidisciplinary discussions regarding unclear etiology of distal CBD obstruction and extensive discussion with patient and family, the decision was made to perform a Whipple procedure for diagnosis and definitive treatment. Intraoperatively, choledochoscopy was performed, which showed very thick yellow mucus and frond-like mucosa near the ampulla. Final pathology showed a 2.0 × 1.5 × 0.5 cm3 granular lesion in the distal CBD. There was prominent biliary epithelial proliferation with tubular–papillary architecture and minimal nuclear atypia in association with chronic inflammation, stroma reaction and smooth muscle proliferation. The overall histological change in the distal CBD resembled that of AH seen in gallbladder, likely non-neoplastic change (Figs 4 and 5). At 1 year follow-up, he is doing well and his jaundice has resolved.

CT of the abdomen and pelvis showing severely dilated intra and extrahepatic bile ducts.

Repeat endoscopy 1 week after ERCP with sphincterotomy and stent placement shows thick mucus obstructing CBD.

Gross pathology showing granular lesion of distal CBD, normal pancreatic duct, no mass in pancreas or papilla of Vater.
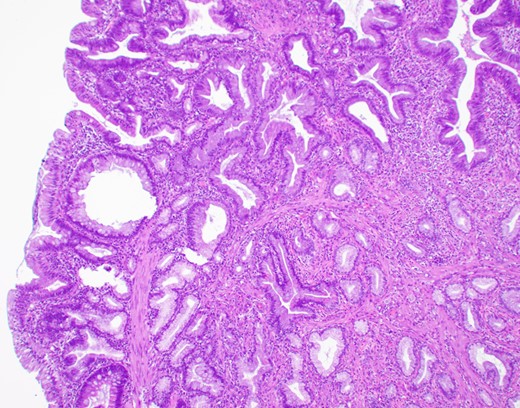
Microscopic appearance (H&E, ×20). Hyperplastic surface epithelium with myofibroblastic stromal proliferation.
DISCUSSION
Benign neoplasms and tumor-like lesions of extrahepatic bile duct are uncommon and it is often difficult to establish a diagnosis before surgical excision. AH is commonly found in the gallbladder and is considered a tumor-like inflammatory lesion. It is characterized microscopically by proliferation of epithelium and smooth muscle. The surrounding glands are usually dilated and filled with mucin, the stroma is generally infiltrated with cells of chronic inflammation [10]. It is extremely rare in the extrahepatic bile duct. This is the 16th case reported in the English literature to date.
Of the reported cases of AH of the extrahepatic bile duct, the ratio of female to male was 12:4. Median age was 62 and mean age was 60 (range: 31–82 years old). The most common chief complaint was abdominal pain, four lesions were located in the proximal bile duct, six were in the middle CBD and six were in the distal CBD. In only one case was there a preoperative diagnosis of adenoma from ERCP biopsy and six cases had negative preoperative cytology and/or biopsy. The surgical procedure performed was local excision in eight and Whipple procedure in seven (Table 1) [1–9].
| Sex . | Age . | Location in bile duct . | Chief complaint . | Preoperative diagnosis . | Type of surgery performed . | Reference . | Year reported . |
|---|---|---|---|---|---|---|---|
| Female | 38 | Middle | Jaundice | Not performed | Local excision | Dowdy | 1965 |
| Female | 62 | Upper | Weight loss | Not performed | Local excision | Burhans | 1971 |
| Female | 82 | Middle | Abdominal pain | Not performed | Local excision | Cook | 1988 |
| Male | 52 | Lower | Abdominal pain | Not performed | Whipple | Ikei | 1989 |
| Female | 55 | Midldle | Abdominal pain | Not performed | Local excision | Legakis | 1990 |
| Male | 75 | Lower | Not described | Not described | Whipple | Matsumoto | 1992 |
| Female | 54 | Upper | Asymptomatic | Not performed | Local excision | Imai | 1995 |
| Female | 69 | Middle | Asymptomatic | Adenoma | Local excision | Lauffer | 1998 |
| Female | 31 | Middle | Abdominal pain | Not performed | Local excision | Tsukamoto | 1999 |
| Female | 64 | lower | Abdominal pain | Not performed | Whipple | Ojima | 2000 |
| Female | 64 | Upper | Asymptomatic | Negative cytology | Local excision | Sato | 2000 |
| Female | 71 | Lower | Abdominal pain | Negative cytology | Whipple | Aoun | 2005 |
| Female | 62 | Lower | Asymptomatic | Negative cytology | Whipple | Iwaki | 2008 |
| Male | 54 | Middle | Jaundice | Negative cytology | Local excision | Numata | 2011 |
| Male | 64 | Upper | Abdominal pain | Negative cytology | Local excision and left hepatectomy | Jakhete | |
| Male | 63 | Lower | Jaundice | Negative cytology and biopsy | Whipple | Present case | 2018 |
| Sex . | Age . | Location in bile duct . | Chief complaint . | Preoperative diagnosis . | Type of surgery performed . | Reference . | Year reported . |
|---|---|---|---|---|---|---|---|
| Female | 38 | Middle | Jaundice | Not performed | Local excision | Dowdy | 1965 |
| Female | 62 | Upper | Weight loss | Not performed | Local excision | Burhans | 1971 |
| Female | 82 | Middle | Abdominal pain | Not performed | Local excision | Cook | 1988 |
| Male | 52 | Lower | Abdominal pain | Not performed | Whipple | Ikei | 1989 |
| Female | 55 | Midldle | Abdominal pain | Not performed | Local excision | Legakis | 1990 |
| Male | 75 | Lower | Not described | Not described | Whipple | Matsumoto | 1992 |
| Female | 54 | Upper | Asymptomatic | Not performed | Local excision | Imai | 1995 |
| Female | 69 | Middle | Asymptomatic | Adenoma | Local excision | Lauffer | 1998 |
| Female | 31 | Middle | Abdominal pain | Not performed | Local excision | Tsukamoto | 1999 |
| Female | 64 | lower | Abdominal pain | Not performed | Whipple | Ojima | 2000 |
| Female | 64 | Upper | Asymptomatic | Negative cytology | Local excision | Sato | 2000 |
| Female | 71 | Lower | Abdominal pain | Negative cytology | Whipple | Aoun | 2005 |
| Female | 62 | Lower | Asymptomatic | Negative cytology | Whipple | Iwaki | 2008 |
| Male | 54 | Middle | Jaundice | Negative cytology | Local excision | Numata | 2011 |
| Male | 64 | Upper | Abdominal pain | Negative cytology | Local excision and left hepatectomy | Jakhete | |
| Male | 63 | Lower | Jaundice | Negative cytology and biopsy | Whipple | Present case | 2018 |
| Sex . | Age . | Location in bile duct . | Chief complaint . | Preoperative diagnosis . | Type of surgery performed . | Reference . | Year reported . |
|---|---|---|---|---|---|---|---|
| Female | 38 | Middle | Jaundice | Not performed | Local excision | Dowdy | 1965 |
| Female | 62 | Upper | Weight loss | Not performed | Local excision | Burhans | 1971 |
| Female | 82 | Middle | Abdominal pain | Not performed | Local excision | Cook | 1988 |
| Male | 52 | Lower | Abdominal pain | Not performed | Whipple | Ikei | 1989 |
| Female | 55 | Midldle | Abdominal pain | Not performed | Local excision | Legakis | 1990 |
| Male | 75 | Lower | Not described | Not described | Whipple | Matsumoto | 1992 |
| Female | 54 | Upper | Asymptomatic | Not performed | Local excision | Imai | 1995 |
| Female | 69 | Middle | Asymptomatic | Adenoma | Local excision | Lauffer | 1998 |
| Female | 31 | Middle | Abdominal pain | Not performed | Local excision | Tsukamoto | 1999 |
| Female | 64 | lower | Abdominal pain | Not performed | Whipple | Ojima | 2000 |
| Female | 64 | Upper | Asymptomatic | Negative cytology | Local excision | Sato | 2000 |
| Female | 71 | Lower | Abdominal pain | Negative cytology | Whipple | Aoun | 2005 |
| Female | 62 | Lower | Asymptomatic | Negative cytology | Whipple | Iwaki | 2008 |
| Male | 54 | Middle | Jaundice | Negative cytology | Local excision | Numata | 2011 |
| Male | 64 | Upper | Abdominal pain | Negative cytology | Local excision and left hepatectomy | Jakhete | |
| Male | 63 | Lower | Jaundice | Negative cytology and biopsy | Whipple | Present case | 2018 |
| Sex . | Age . | Location in bile duct . | Chief complaint . | Preoperative diagnosis . | Type of surgery performed . | Reference . | Year reported . |
|---|---|---|---|---|---|---|---|
| Female | 38 | Middle | Jaundice | Not performed | Local excision | Dowdy | 1965 |
| Female | 62 | Upper | Weight loss | Not performed | Local excision | Burhans | 1971 |
| Female | 82 | Middle | Abdominal pain | Not performed | Local excision | Cook | 1988 |
| Male | 52 | Lower | Abdominal pain | Not performed | Whipple | Ikei | 1989 |
| Female | 55 | Midldle | Abdominal pain | Not performed | Local excision | Legakis | 1990 |
| Male | 75 | Lower | Not described | Not described | Whipple | Matsumoto | 1992 |
| Female | 54 | Upper | Asymptomatic | Not performed | Local excision | Imai | 1995 |
| Female | 69 | Middle | Asymptomatic | Adenoma | Local excision | Lauffer | 1998 |
| Female | 31 | Middle | Abdominal pain | Not performed | Local excision | Tsukamoto | 1999 |
| Female | 64 | lower | Abdominal pain | Not performed | Whipple | Ojima | 2000 |
| Female | 64 | Upper | Asymptomatic | Negative cytology | Local excision | Sato | 2000 |
| Female | 71 | Lower | Abdominal pain | Negative cytology | Whipple | Aoun | 2005 |
| Female | 62 | Lower | Asymptomatic | Negative cytology | Whipple | Iwaki | 2008 |
| Male | 54 | Middle | Jaundice | Negative cytology | Local excision | Numata | 2011 |
| Male | 64 | Upper | Abdominal pain | Negative cytology | Local excision and left hepatectomy | Jakhete | |
| Male | 63 | Lower | Jaundice | Negative cytology and biopsy | Whipple | Present case | 2018 |
No radiologic study has been shown to distinguish AH from cancer of the extrahepatic bile duct or papilla of Vater. Abdominal CT can show the lesion to be either heterogeneous or homogeneous low-attenuating mass with dilation of the proximal bile duct [6]. Brushings and biopsies also do not lead to a preoperative diagnosis. In only one of the reported cases, preoperative biopsy by ERCP showed adenoma. In our case, multiple attempts at diagnosis were made with brushings, FNAB, and even cold forceps biopsy. However, these failed to yield a preoperative diagnosis.
AH of the extrahepatic bile duct can cause biliary obstruction and in our case acute cholangitis. Three of the reported cases presented with jaundice. In our case, because of the difficulty in diagnosis and the persistent and recurrent obstruction of the bile duct, a Whipple procedure was performed. This patient had a good outcome and is doing well one year postoperatively.
In conclusion, AH is extremely rare and diagnosis is very difficult. It is a benign process, but often requires a major operation to definitively diagnose.
CONFLICT OF INTEREST STATEMENT
None declared.



