-
PDF
- Split View
-
Views
-
Cite
Cite
Marina Raguž, Yannick Mudrovčić, Domagoj Dlaka, Fadi Almahariq, Dominik Romić, Čedna Tomasović-Lončarić, Danko Müller, Petar Marčinković, Anđelo Kaštelančić, Darko Chudy, Primary dural lymphoma mimicking meningioma: a clinical and surgical case report, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy189, https://doi.org/10.1093/jscr/rjy189
Close - Share Icon Share
Abstract
Introduction: Primary central nervous system lymphoma and its subtype, primary dural lymphoma, are types of non-Hodgkin's lymphoma that only occur in the central nervous system without any dissemination. They are extremely rare cases of extra nodal lymphomas accounting for 1--5% of intracranial tumors. Case report: We present a patient diagnosed with primary dural lymphoma in right frontal brain region who underwent surgical resection. Histopathological analysis revealed diffuse B-type large cell non-Hodgkin lymphoma. Patient underwent four cycles of R-CHOP and intrathecal methotrexate protocol. Six months postoperative, no signs of newly onset infiltration were present. Discussion: Primary dural lymphoma most likely presents with unusual radiological signs, which can easily be mistaken for meningioma, the main differential diagnosis. A thorough immunological, histopathological and clinical patients profile should be conducted in order to establish the certainty of diagnosis. Although there are few treatment options: surgery, radiotherapy or chemotherapy, there is no established treatment protocol.
INTRODUCTION
Primary dural lymphoma (PDL) is a subtype arising from a larger group called primary central nervous system lymphomas (PCNSL). PCNSL are extra nodal non-Hodgkin lymphomas originating from the brain, meninges or spinal cord, but in the absence of systemic involvement [1]. This pathology is accounted for less than 1% of all central nervous system (CNS) lymphomas and <0.1% of all non-Hodgkin’s lymphomas generally [2]. The real occurrence of PDL is not yet known. Two largest series describing PDL had only 8 and 15 patients [3, 4].
Lymphomas can be roughly divided based on arising site into nodal and extra nodal. PDL arises from the dura mater and belongs to the low-grade B-cell marginal zone group of tumors which is non-specific for CNS pathologies which are mostly high-grade diffuse large B-cell lymphomas [1]. Marginal zone lymphomas are a torpid non-Hodgkin type of lymphoma and they occur more frequently in the gastrointestinal system (MALT lymphomas) [1, 4]. Usually the preferential site of dissemination for MALT lymphomas is within other organs of MALT system, but they can also be noticed in non-gastrointestinal tissue such as skin, salivary glands [5]. One of their characteristics is a localized disease, just like PDL, which shares a lot of features with marginal zone B-cell lymphomas.
CASE REPORT
A 34-year-old male patient was presented with a 2-month history of intermittent headaches in the right frontal region. No other significant neurological deficits were found. Initial magnetic resonance imaging (MRI) revealed mass in the right frontal part of the skull (Fig. 1). The mass was attached to dura mater and it was mildly compressing the middle frontal gyrus beneath. Also, signs of intraosseal propagation were present. Patient underwent right side frontal craniectomy. Bone attached to the tumor was extracted. Duroplasty and cranioplasty were performed. Surgery went without complications. Postoperative computerized tomography (CT) was satisfying. Tissue samples from multiple sites of tumor connected to dura with surrounding bone were taken intraoperatively and underwent histopathological analysis. Tumor consists of large cells with pleomorphic nuclei and prominent nucleoli, with pathological mitotic figures. Tumorous tissue shows immunohistological reactivity for CD45 LCA, CD20, CD79a, CD10, BCL6 and PAX5. They were partly positive for BCL2 and CD30 and negative for CD3 and CD21. C-myc shows positivity in 36% of tumor cells. Proliferation index Ki67 is diffusely 75% (Fig. 2). According to WHO classification it corresponds to diffuse large B-cell lymphoma. Afterwards, extended diagnostics were performed. Bone marrow biopsy showed an abnormality in the percentage of non-segmented neutrophils of 17%. Other results showed medium–high erythropoiesis with normal cell ratios but without findings of malignant alteration or infiltration. A cylindrical sample showed no morphological nor immunohistochemical (CD20, PAX5, Ki67 and CD3) evidence of malignant infiltration. Lumbar puncture was also performed and cerebrospinal fluid (CSF) samples showed no positivity to malignant cells. Afterwards, full body CT was performed, followed by ultrasound including thyroid and salivary glands. Also, MRI of brain and spinal cord was done. All conducted imaging methods revealed normal anatomical and structural features without traces of lymph node enlargement or flee fluid throughout the body. A hematologist was consulted and methotrexate or R-CHOP therapy was recommended.
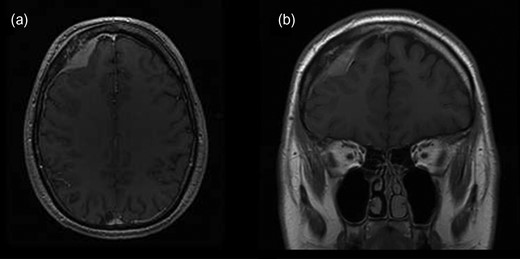
Initial brain MRI showing extra-axial mass in the right frontal part of anterior cranial fossa in (a) transverse and (b) coronal plain.
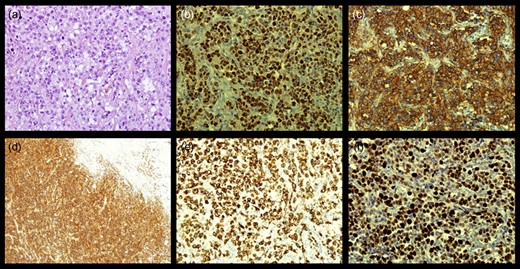
Microphotography of tumorous tissue with fibrous tissue of dural origin on the edge of the surgical material, measuring together 5 cm in greatest diameter: (a) hemalaun eosin staining, magnification of ×400; (b) immunohistological reactivity BLC6, magnification of ×400; (c) immunohistological reactivity CD20, magnification of ×400; (d) immunohistological reactivity CD45 LCA, magnification of ×100; (e) immunohistological reactivity CD79, magnification of ×400; and (f) proliferation index Ki67, magnification of ×400.
The patient was transferred to the hematology department for further diagnostic procedures. Upon analysis no pathological findings were found. After consultation R-CHOP and intrathecal methotrexate protocol was chosen. The patient was administered four cycles of R-CHOP and intrathecal methotrexate. Four months afterwards, MRI and neurosurgical control were performed. MRI revealed satisfying postoperative result without any new intracranial masses (Fig. 3).
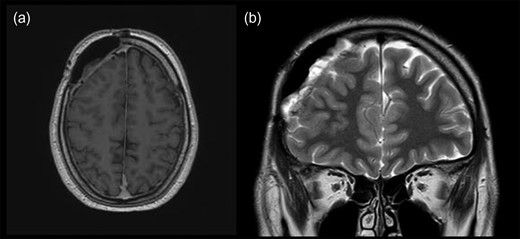
MRI scans of brain, 4 months postoperatively, revealing no recurrence of lymphoma in (a) transverse and (b) coronal plain.
DISCUSSION
Meningeal involvement of lymphoma as a result of a systemic disease can occur extremely rare. For patients with PDL the most predominant histopathological finding is marginal zone B-cell lymphoma, frequently found in the GI system as mucosa associated lymphoid tissue [4].
When suspecting a PCNSL, of primary importance is CT and MRI, especially contrast enhanced MRI, because differential diagnosis with the highest level of importance is meningioma [1, 2, 6]. Other differential diagnoses include dural metastasis, fibrous tumors, gliosarcomas, leiomyosarcomas or neurosarcoidosis [1, 3]. MRI reveals single or multiple extra-axial masses; mostly more than one mass. Perilesional edema is usually not excessive and mainly depends on mass size and location. Respectively, cerebral convexities are the most common site of involvement, but other sites such as falx, tentorium and sellar or suprasellar regions can be affected. Since the most common site of masses is cerebral convexity, intraoseal propagation occasionaly occurs [1].
More rarely, intraventricular and spine located masses can be found. Lumbar puncture as well as CSF cytology and flow cytometry should always be performed, respectively. A thorough analysis of the CSF should be done to minimalize the possibility of free floating tumor cell seeding and to perform evaluation of the intradural space.
It is yet to be understood the biological basis of the dural space involvement. Due to scarce materials and its rarity, the mechanism of PCNSL malignant transformation point of access in the CNS and origin of malignant cells are insufficiently known. Outside the CNS, marginal zone B-cell lymphomas are believed to derive from inflammation processes due to infectious organisms or autoimmune diseases which tends to open the question of infectious or autoimmune co-etiology in PCNSL [4]. Also worth mentioning is the fact that dura is outside the blood–brain barrier and this increases the risk of PDL systemic relapse.
Different drugs and procedures were tried out, such as complete surgical resection, systematic or intrathecal chemotherapy with CHOP, rituximab, methotrexate, alkylating agents, cytarabine and vincristine [1, 6]. Methotrexate based approach in treating primary lymphomas is the most effective way, especially when combined with brain irradiation; the survival rates are around 70% [1]. PDL tends to respond positively to surgery and radiotherapy. They are preferable choices due to its indolent character and high radio sensitivity but requires relatively low doses of radiotherapy [1, 3]. Although there are limited reports and PDL is quite rare, further investigations in this field are required in order to develop the most effective treatment option.
CONFLICT OF INTEREST STATEMENT
On behalf of all authors, the corresponding author states that there is no conflict of interest.
COMPLIANCE WITH ETHICAL STANDARDS
Patient has given informed consent for participation in this article.



