-
PDF
- Split View
-
Views
-
Cite
Cite
Fabiola Aguilera, Tajudeen O Dabiri, Daniel T Farkas, Pneumoperitoneum caused by tubo-ovarian abscess in an elderly patient, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy191, https://doi.org/10.1093/jscr/rjy191
Close - Share Icon Share
Abstract
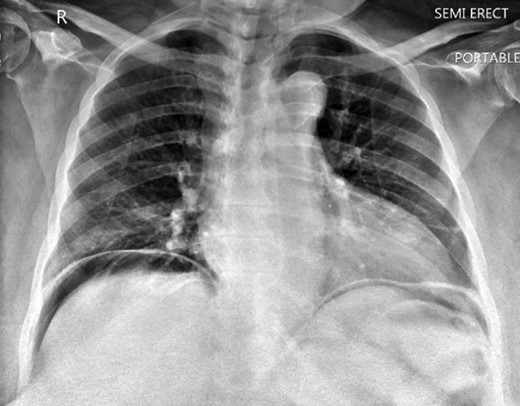
Perforation of the gastrointestinal tract may present with abdominal pain and imaging demonstrating pneumoperitoneum. These findings usually require exploratory laparotomy for diagnosis and treatment. Tubo-ovarian abscess (TOA) is a complication of pelvic inflammatory disease presenting as an encapsulated inflammatory mass, but it can occasionally involve other pelvic organs. TOA is most commonly seen in females of reproductive age. Here we report a case of a 63-year-old female presenting with abdominal pain, fever and vomiting. Chest x rays and computed tomography scan revealed pneumoperitoneum. Emergent exploratory laparotomy was performed, and the findings were consistent with TOA and intact bowel. The patient recovered well after surgery with antibiotic therapy. In conclusion, while pneumoperitoneum is mostly caused by perforation of the gastrointestinal tract, other possibilities such as gynecological complications should be considered.
INTRODUCTION
Perforated viscous leading to spillage of intra-luminal contents into the peritoneum and secondary sepsis, generally requires an emergent exploratory laparotomy to make the diagnosis and for treatment. This pathologic process is suspected with a patient complaining of abdominal pain with peritoneal signs and diagnostic imaging of extra-luminal air in the abdomen. Tubo-ovarian abscess (TOA) is usually an encapsulated infectious inflammatory process involving the fallopian tube and the ovary, but could also involve other pelvic organs. It is usually treated with antibiotics requiring surgical intervention in only 25% of the cases [1]. In a Medline search only two cases have been described in patients with TOA and pneumoperitoneum taken to the operating room for exploratory laparotomy under the impression of possible perforated viscous [2, 3]. Both of these patients were in their third decade of life. This is the first one case reported in an elderly patient.
CASE REPORT
A 63-year-old African American female presented with complaints of abdominal pain located more in the right lower quadrant and multiple episodes of vomiting for the past 4 days. She had a history significant for ventral hernias and past surgical history of two myomectomies. Physical exam demonstrated right upper and right lower abdominal tenderness and peritoneal signs. Patient had fever and tachycardia. Chest x ray showed free air under the diaphragm (Fig. 1). Computer tomography revealed pneumoperitoneum and alarge gas containing collection in the pelvis measuring 13.6 × 8.8 cm2. This was in close proximity to the sigmoid colon which appeared thickened, and extending to the right adnexal region (Fig. 2A and B). Laboratory results showed white blood cell count 28.7 × 103/ μL, 93% neutrophils. The patient was taken to the operating room for exploratory laparotomy with the presumptive diagnosis of perforated sigmoid diverticulitis.
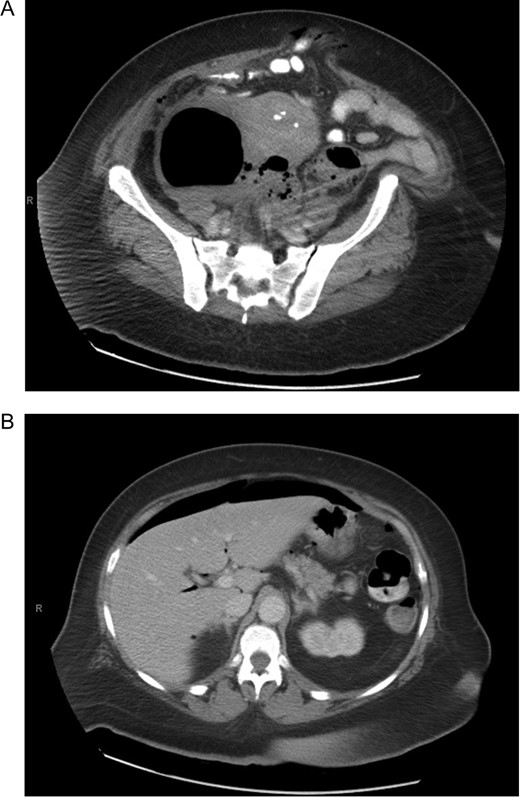
(A) Computer tomography showing pelvic collection. (B) Computer tomography showing pneumoperitoneum.
Intra-operatively the collection was identified as a TOA, with no evidence for bowel perforation. The uterus was large with fibroids, with inflammatory tissue and abscess in both adnexa, but more so on the left. The abscess cavity extended to the anterior surface of the sigmoid, but the bowel appeared normal with no evidence of diverticulitis or perforation. The abscess was drained, and a supra-cervical hysterectomy and bilateral salpingo-oophorectomy was performed. This was done through a midline incision, and her recurrent incarcerated incisional hernias were repaired primarily as well.
Pathology specimen revealed a right TOA with cystic changes and inflammation (foreign body giant reaction). Tissue cultures showed growth of skin flora microorganisms. She was treated with antibiotic therapy to cover pelvic inflammatory disease. Her postoperative course was uneventful and she was discharged on postoperative Day 11. She was followed in the clinic and recovered well, with no sign of recurrent abscess after 3 months of follow-up.
DISCUSSION
Pneumoperitoneum is most commonly associated with perforated gastrointestinal tract, requiring surgical exploration. Non-surgical causes of pneumoperitoneum are also known such us mechanical ventilation, percutaneous gastrostomy placement, paracentesis, peritoneal dialysis, vaginal instrumentation, bacterial peritonitis, pulmonary abscess and ruptured pulmonary alveoli. TOA is a serious gynecological infection presenting as a mass in the adnexa. It is rare to see gas in TOA but it has been reported in the literature [4]. Chang et al. [2] presented a patient with pneumoperitoneum mistakenly taken to the operating room under the impression of perforated bowel with intra-operative finding of TOA similar to the case that we are presenting. Their culture of fluids revealed growth of Escherichia coli. Landers and Sweet [5] described that most cases of TOA are caused by anaerobic organisms, including the resistant gram-negative anaerobes such as Bacteroides fragilis and Bacteroides bivius. In our case we think that even though there was growth of skin flora on aerobic media, an anaerobic organism was most likely the cause of the infection.
Initial management of TOA is antibiotic therapy, however, if there is not clinical improvement within 2–3 days, surgical intervention should be considered. An indication for immediate operation is the suspicion of rupture TOA or patients potentially developing septic shock [5, 6].
In conclusion, although this is rare in elderly patients, the diagnosis of TOA is possible in cases of pneumoperitoneum with a gas containing collection in the pelvis.
CONFLICT OF INTEREST STATEMENT
None of the authors have conflicts of interest to declare.
FUNDING
This project received no funding.
REFERENCES
- abdominal pain
- computed tomography
- fever
- intestines
- reproductive physiological process
- surgical procedures, operative
- vomiting
- diagnosis
- diagnostic imaging
- pelvis
- pneumoperitoneum
- chest
- pelvic inflammatory disease
- tubo-ovarian abscess
- antibiotic therapy
- gastrointestinal tract
- older adult
- laparotomy, exploratory



