-
PDF
- Split View
-
Views
-
Cite
Cite
Andreas Kiriakopoulos, Dimitrios Linos, Thyroid paraganglioma: a case series of a rare head and neck tumor, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy184, https://doi.org/10.1093/jscr/rjy184
Close - Share Icon Share
Abstract
Thyroid paragangliomas are rare neuroendocrine tumors. We present two cases analyzing their clinical presentation and pathology findings. A 44-year-old woman presented with a 33 mm left thyroid lobe mass. A 27-year-old male presented with a 27-mm right thyroid lobe mass and a FNA biopsy suggesting a follicular thyroid tumor. Both patients underwent total thyroidectomy. Vigorous bleeding was noted on the first case. Histologic sections revealed encapsulated tumors, whereas immunochemical stains were positive for chromogranin A, synaptophysin and NSE and negative for thyroglobulin, calcitonin, CEA and S-100. After an 18- and 12-month follow-up, respectively, both patients have no signs of local recurrence or distant metastasis. Preoperative diagnosis of thyroid paragangliomas was never attained in this series. Immunohistochemistry is mandatory for proper differential diagnosis. For the surgeon, the operation is technically demanding mainly due to the increased vascularity and friability of the tumor.
INTRODUCTION
Paragangliomas are rare extra-adrenal neuroendocrine tumors derived from the neural crest. Parasympathetic paragangliomas are almost exclusively present in the head and neck region [1, 2] and include the extremely rare primary thyroid paraganglioma [3].
Surgical removal of thyroid paragangliomas is the mainstay of treatment. Its identification and differential diagnosis from other thyroid tumors is extremely important in terms of subsequent management and prognosis [3, 4]. We describe herein two cases of primary thyroid paragangliomas.
CASE SERIES REPORT
Case 1
A 44-year-old woman with an unremarkable family and past medical history was referred due to an AUS/FLUS (Bethesda category III), 33 mm nodule on the upper pole of the left thyroid lobe. On cervical U/S, the nodule exhibited a heterogeneous pattern with cystic/solid features and a markedly increased intra-nodular vascular flow without microcalcifications or central/lateral lymph node involvement. Thyroid function tests and calcitonin levels were normal. During the operation the tumor was friable and densely adherent to the surrounding tissues leading to vigorous bleeding. After a total thyroidectomy the patient was discharged the next day in excellent condition.
Histologic examination showed a 34 × 26 mm tumor on the left lobe which consisted of neoplastic cells nests arranged in a characteristic ‘zellballen’ pattern (Figs 1 and 2). Immunohistochemistry was positive for neuroendocrine markers (Chromogranin A, Synaptophysin, CD56, NSE, CD 57) and negative for cytokeratins (AE1/AE3, 7, 8, 19), Calcitonin, CEA and Thyroglobulin (Figs 3–5).
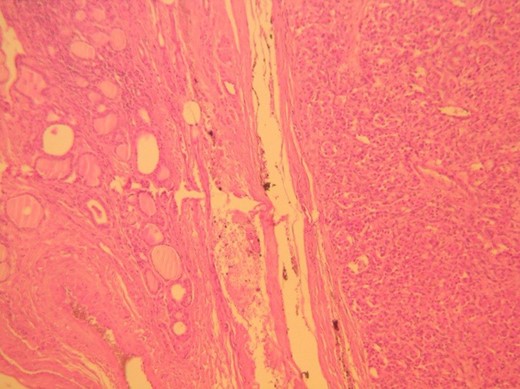
H&E ×100, original magnification. Tumor is shown to the right, circumscribed and surrounded by a thin fibrous capsule (arrows).
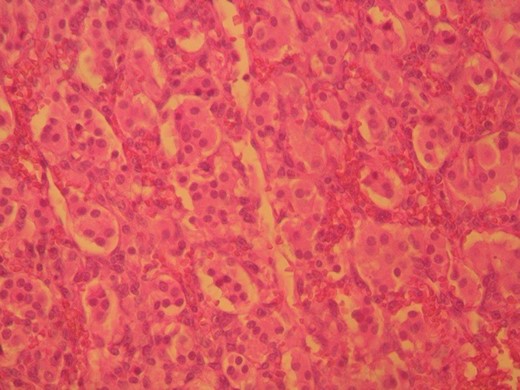
H&E ×400, original magnification. The tumor shows the characteristic ‘zellballen’ pattern.
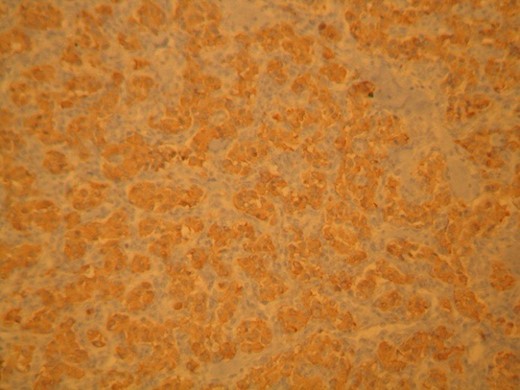
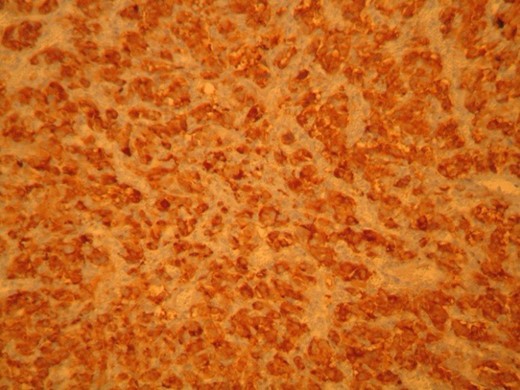
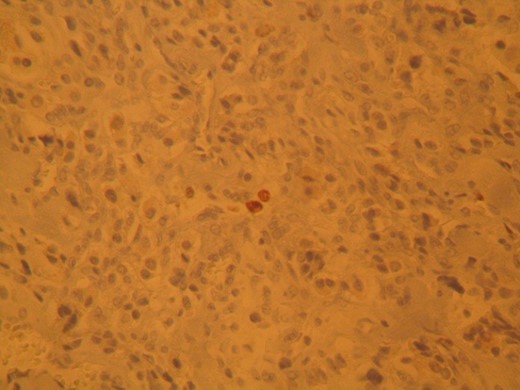
Thyroid paraganglioma, Ki67 proliferation marker. Positivity of occasional neoplastic cells.
Case 2
A 27-year-old man with an unremarkable family and past medical history was referred due to a 27 mm solitary nodule of the right thyroid lobe. Preoperative ultrasound showed a heterogeneous mass with increased intra-nodular vascular flow, whereas the FNA biopsy set the suspicion of a thyroid follicular tumor. Thyroid function tests and calcitonin levels were normal. Histologic sections revealed a well-circumscribed, solid tumor with inconsistent capsule. Immunohistochemical stains were positive for chromogranin A and Synaptophysin but negative for Thyroglobulin, cytokeratins-7, 8, 19, Calcitonin, CEA, CD56 and S-100, consisted with the diagnosis of thyroid paraganglioma.
Both patients, soon after the diagnosis, were evaluated for cathecholamines overproduction that was negative and underwent a full imaging investigation including neck, thoracic and abdominal CTs that revealed no synchronous tumors. Additionally, they were enrolled in a follow-up scheme that included neck U/S twice annually for the first 2 years and then one per year for the next 3 years. On the first year postoperatively, cervical U/S in both patients showed no signs of local or locoregional recurrence and after 5 years for the first patient and 3 years for the second, both remain disease free.
DISCUSSION
Paragangliomas are rare extra-adrenal chromaffin tumors derived from neural-crest derived cells located at sympathetic or parasympathetic paraganglia, the latter being present, in the vast majority, in the head and neck region [1, 2]. Carotid body tumors, jugular paragangliomas and tympanic paragangliomas account for 80% of all head and neck paragangliomas [5] with vagal paragangliomas accounting for another 5% [6]. Nasal, orbital, laryngeal and other paragangliomas occur much less frequently.
At least 30% of all Pheochromocytomas/Paragangliomas are hereditary and harbor germline mutation in 1 of the 10 identified susceptibility genes: RET, NF1, VHL, SDHAF2, TMEM127 or MAX, and in genes encoding the four subunits of succinate dehydrogenase complex [7]. SDHD at chromosome 11q23, SDHB at chromosome 1p36, SDHC at chromosome 11q23 and SDHAF2 have all been implicated in the pathogenesis of head and neck paragangliomas [7].
Thyroid paragangliomas are exceptionally uncommon and show a strong female preponderance typically appearing between 40 and 60 years of age. They present as asymptomatic, solitary thyroid nodules. The preoperative diagnosis is difficult since the cytologic and histologic features may overlap with other, more common primary thyroid neoplasms such as medullary thyroid carcinoma, thyroid neuroendocrine tumor and thyroid trabecular adenomas [8]. Preoperative U/S may reveal the presence of a hypervascular thyroid nodule. Surgical removal may be hazardous due to the increased vascularity and friability of the tumor which may also be densely adherent to the surrounding tissues. Histologic diagnosis of a thyroid paraganglioma is important since it denotes a mostly benign behavior with no reported distant metastases, whereas thyroid medullary carcinoma is clearly a malignant tumor with considerable metastatic potential [8]. Immunohistochemistry panel including chromogranin A, Synaptophysin, NSE, Thyroglobulin, CT, CEA, CD56, Cytokeratins and S-100, is essential for this particular differential diagnosis.
Because of the rarity of these tumors, their clinical behavior and natural history is largely unknown. Even though local aggressiveness with tracheal or recurrent nerve invasion have been reported, thyroid paragangliomas have never been associated with distant metastasis during follow-up periods between 2 months and 8 years [3]. Postoperatively, patients with paragangliomas should undergo hormonal evaluation for functional disease, imaging evaluation for multicentric and metastatic disease, and genetic counseling.
CONFLICT OF INTEREST STATEMENT
None declared.



