-
PDF
- Split View
-
Views
-
Cite
Cite
Luis G Garcia-Herreros, Ernesto Villamizar, Diego F Salcedo, Trans‐mediastinal herniation of pulmonary bulla with paradoxical pneumothorax, Journal of Surgical Case Reports, Volume 2018, Issue 7, July 2018, rjy174, https://doi.org/10.1093/jscr/rjy174
Close - Share Icon Share
Abstract
Trans-mediastinal herniation of a lung bullae is an extremely rare condition. Here we present a case of a 75-year-old patient with a clinical history of chronic obstructive pulmonary disease and emphysema presenting with a right contralateral pneumothorax secondary to a trans-mediastinal herniated lung bullae. Herniation occurred through a mediastinal pleural defect; we call this event a paradoxical pneumothorax. To our knowledge this is the first report in the medical literature. The patient was successfully treated using a VATS approach with a right pleurodesis, a left thoracoscopic trans-mediastinal hernia reduction and bullectomy.
INTRODUCTION
The most common clinical presentation of chronic obstructive pulmonary disease in heavy smoking patients is lung emphysema along with secondary bullous disease. Bullae are thin-walled structures with a diameter larger than 1 cm characterized by the pathologic elongation of air spaces distal to terminal bronchioles associated to alveolar wall destruction [1, 2]. Some bullae can be large enough to cause pulmonary hernias, this is the least frequent cause of lung herniation. The primary cause of secondary spontaneous pneumothoraxes is the rupture of a lung bullae [3]. This results in a surgical emergency since the degree of insult to respiratory function is significant in patients with chronic obstructive pulmonary disease (COPD) [4]. Cases of giant herniated bullae have been reported, however, here we report the first case of a right secondary spontaneous pneumothorax as a result of an incarcerated left trans-mediastinal ruptured lung bullae through a mediastinal pleural defect.
CASE REPORT
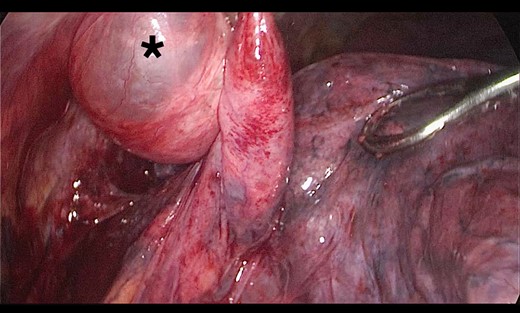
A 73-year-old male patient with a clinical history of COPD, lung emphysema and a 30-year smoking history was admitted to the ED due to a 24-h clinical picture of dyspnea immediately following a sudden bout of dry coughing. Physical examination showed a dyspneic patient, tachypnea of 25 rpm, heart rate of 85 bpm and blood Pressure of 135/75 mmHg along with central cyanosis. Chest exam showed a hyper-resonant right hemithorax along with reduced breath sounds. Initial chest X-ray revealed a large right-sided pneumothorax (Fig. 1). A right chest tube was placed in the ED. Emergency echocardiogram had no significant findings and spirometry showed suspected patterns of obstruction. Following patient stabilization, a high-resolution chest computed tomography (HRCT) was performed revealing extensive pan lobar emphysema throughout both lungs, para septal emphysema in both the anterior upper lobes and herniation of a left lung bullae through the anterior mediastinal pleura along with a right-sided pneumothorax with the chest tube in place with persistent air space (Fig. 2). The patient was taken to surgery where a right video-assisted thoracoscopic (VATS) approach showed severe lung emphysema and a contralateral herniated left lung bulla through the mediastinal pleura anterior to the pericardium (Fig. 3). Right pleurodesis was performed using Talc and a left posterior thoracoscopy showed a severe emphysematous left lung with a lingular herniated bulla to the right hemithorax through an anterior mediastinal pleural defect along with pleural adhesions (Figs 4 and 5). Thoracoscopic hernia reduction was performed along with bullectomy using 60 mm mechanical sutures (Fig. 6). Chest tubes were removed on POD 3 (right) and POD 4 (left). The patient had significant respiratory improvement and was discharged on POD 5.
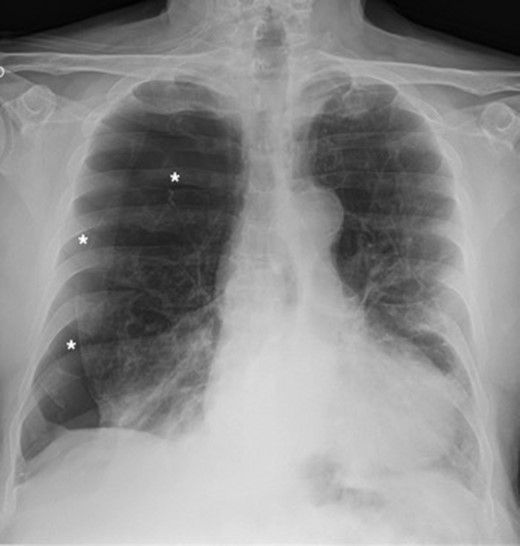
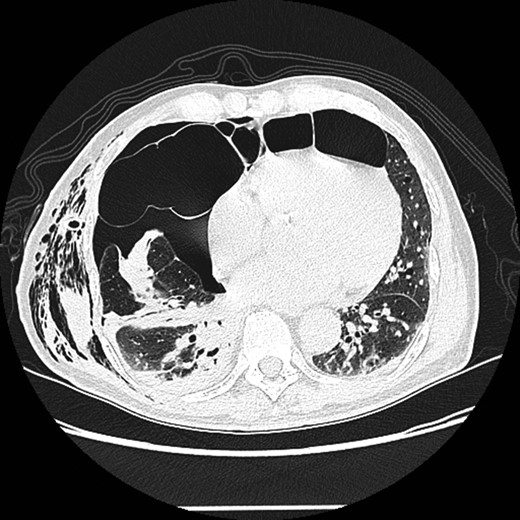
High-resolution computed tomography (HRCT) thorax showing trans‐mediastinal herniation of pulmonary bulla with right pneumothorax.
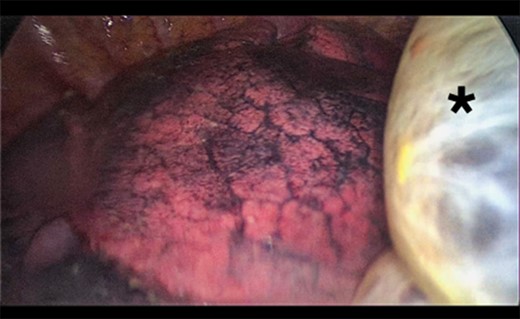
Thoracoscopic view of transmediasinal herniation of pulmonary bulla to the right hemithorax (asterisk).
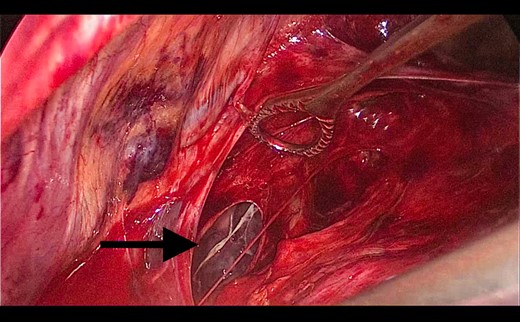
Thoracoscopic view from left side of transmediasinal hernia of pulmonary bulla after reduction (asterisk).
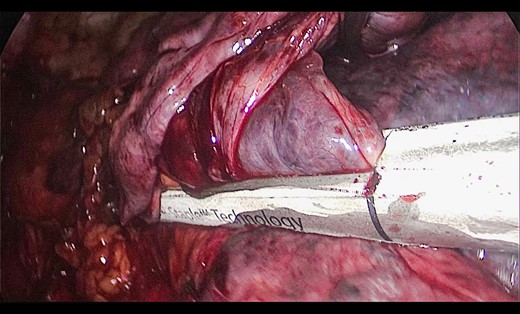
Thoracoscopic view from left side of thoracoscopic bullectomy.
DISCUSSION
A bulla is defined as a pathological 1 cm diameter air filled space within the lung parenchyme typically secondary to lung tissue destruction. Characteristically a bulla has a very thin external wall made up of the visceral pleura and an internal wall consisting of the damaged lung tissue. Most bullae are found in the upper lobes and are typically avascular and do not participate in gas exchange [5]. Most patients with bullae have a significant history of cigarette smoking. Cocaine use, pulmonary sarcoidosis, α-1-antitrypsin deficiency, Marfan syndrome and Ehlers–Danlos syndrome may be associated with emphysematous bullae in a lesser degree [6, 7]. The right and left pleura come into contact with each other at three main anatomical sites where mediastinal herniation is possible when there is increased intrathoracic pressure: anterior to the ascending aorta, immediately behind the heart and below the ascending aorta [8]. Lung bullae can also herniate through the intercostal spaces and through the neck where weakness of the Sibson’s fascia and neck muscles may contribute to cervical herniation of pulmonary bullae [9, 10].
Herniation of an emphysematous bulla is a very rare condition and complication and very few cases are reported. In the English literature, there are only four cases of mediastinal herniated pulmonary bullae reported. None however presented with contralateral pneumothorax (paradoxical pneumothorax) due to the rupture of a trans-mediastinal herniated bullae. The clinical presentation is non-specific, it includes cough, dyspnea, dysphagia and exacerbation of the underlying symptomatology of COPD. Chest X-rays show pneumothorax but does not always identify the trans-mediastinal bulla; diagnosis is thus confirmed with the help of chest tomography confirming the anatomical defects [3]. Surgical intervention is indicated in cases with severe dyspnea and bullae of more than 30% that compress the adjacent lung fields. Surgical resection is also indicated if the bullae is infected or if rupture produces a pneumothorax [10]. We successfully treated our patient with a VATS approach using right talc pleurodesis and left thoracoscopic hernia reduction with bullectomy.
CONFLICT OF INTEREST STATEMENT
None declared.



