-
PDF
- Split View
-
Views
-
Cite
Cite
Jodie Trautman, Brielle E Wood, Steven J Craig, A rare case report of gallbladder carcinosarcoma, Journal of Surgical Case Reports, Volume 2018, Issue 7, July 2018, rjy167, https://doi.org/10.1093/jscr/rjy167
Close - Share Icon Share
Abstract
Introduction:Carcinosarcoma of the gallbladder (CSGB) is a rare clinical condition. To date, only 107 cases of CSGB have been reported worldwide. We present our experience of a late presentation of disseminated CSGB. To this we add a discussion of prognostic factors and treatment options for this rare gallbladder malignancy drawn from CSGB cases reported in the literature. Case report: A 73-year-old female presented to our facility with a poorly differentiated CSGB with widespread liver and peritoneal metastases. Fifteen days from the time of hospital admission, the patient suffered an acute episode of massive haematemesis with clinical signs of perforated viscous. Her cause of death was thought to be a tumour-related duodenal erosion. Discussion: Given the poor prognosis of CSGB, particularly when diagnosed at locally advanced or disseminated stages, we suggest a greater role for laparoscopic tissue diagnosis before considering radical surgical intervention.
INTRODUCTION
Carcinosarcoma of the gallbladder (CSGB) is a rare malignant tumour of the gallbladder. A meta-analysis reported that between 1907 and May 2007, 68 cases of CSGB were identified in the world literature [1]. An online search of the PubMed database using terms ‘carcinosarcoma’ AND ‘gallbladder’, ‘sarcomatoid carcinoma’ AND ‘gallbladder’, and ‘spindle cell carcinoma’ AND ‘gallbladder’ identified a further 39 reported cases of carcinosarcoma between June 2007 and December 2017. Thus, to date, a total of 107 cases of CSGB have been presented in the published literature. To that tally, we add an additional case of CSGB in a patient who presented to and was managed in a public hospital in New South Wales, Australia.
CASE REPORT
A 73-year-old female presented to our facility with a 1-week history of abdominal distension, constipation, nausea and vomiting. She had lost 13 kg of weight in the preceding 6 months. The patient had a background medical history that was significant for hepatitis C, treatment for which had been completed 5 months earlier. She also suffered from gastro-oesophageal reflux disease and chronic constipation. She was an ex-smoker with a 40-pack-year history, did not drink alcohol and had recently migrated to Australia from Brazil.
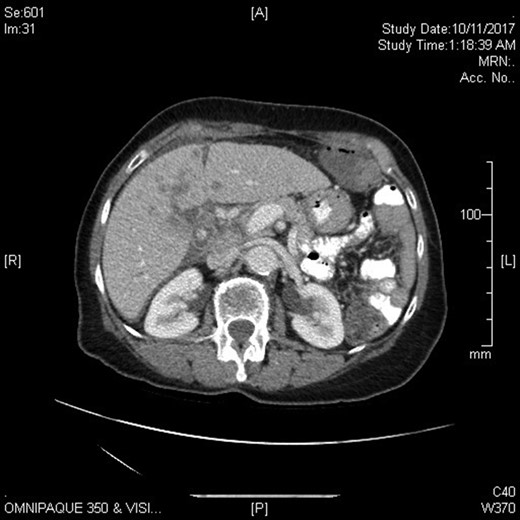
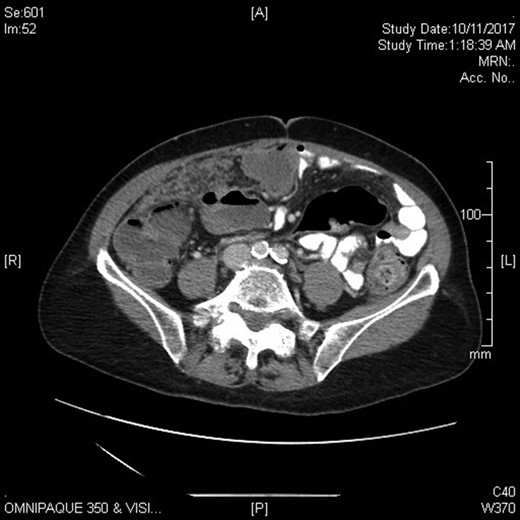
Physical examination revealed a markedly distended abdomen that was otherwise soft and non-tender. She had liver enzymes that were elevated two to five times the upper normal limit. Her tumour markers showed mildly elevated CA-125 and BetaHCG, but normal CEA, AFP and CA19.9. Computed tomography imaging revealed stigmata of chronic cholecystitis and a mass at the gallbladder fossa with evidence of hepatic and peritoneal metastases. The overall appearance was suggestive of metastatic gallbladder carcinoma, though primary hepatocellular carcinoma was considered a possibility given her past history of hepatitis C (Figs 1 and 2).
A diagnostic laparoscopy was performed to quickly and safely obtain a tissue diagnosis. The gallbladder was white, nodular and firm with widespread metastatic disease involving the liver, bowel, omentum and peritoneum. Multiple biopsies were taken of liver nodules, peritoneal and omental deposits. Histopathology showed a poorly differentiated malignant tumour suggestive of sarcomatoid carcinoma. The tumour consisted of fascicles of malignant spindle cells with atypical nuclei and frequent mitoses. Immunohistochemistry stains were positive for AE1/AE3, Cam 5.2, Desmin, SMA and negative for CK7, CK20, CDX2, CD31, CD10, P40, PAX8, GATA3, TTF1, WT1.
Fifteen days from the time of hospital admission, whilst awaiting transfer to a palliative care facility, the patient suffered an acute episode of massive haematemesis with clinical signs of perforated viscous. Her cause of death was thought to be a tumour-related duodenal erosion.
DISCUSSION
CSGB is a mixed tumour with epithelial and mesenchymal components. The meta-analysis by Zhang et al. [1] and the subsequent reported cases, reveal the most common epithelial component to be adenocarcinoma and the most common mesenchymal component spindle-shaped cells. CSGB has a female to male ratio of 2.7:1. It presents most commonly with abdominal pain as well as anorexia, weight loss, lethargy, vomiting and jaundice [2, 3]. Serum investigations, including inflammatory markers, liver function tests and tumour markers are nonspecific and often within normal limits [4]. Imaging usually identifies an intraluminal polypoid gallbladder mass. Features that will assist in differentiating CSGB from other gallbladder tumours are reported to include calcification within the tumour on computed tomography [4], preservation of gallbladder shape despite the large tumour size on ultrasonography [5], and variations in intensity on T2-weighted magnetic resonance images that provide qualitative information about the tumour components [6].
The median survival for CSGB is 5 months from the time of diagnosis [1, 3]. Factors that predict a more favourable prognosis include tumour size being <5 cm [1], the appearance of early stage disease (Stage I or Stage II according to AJCC or UICC classifications), and curative resection. The presence of gallstones, epithelial and mesenchymal type, age and sex are not prognostic factors [1]. To date, surgical resection has been the treatment of choice for non-disseminated carcinosarcoma. Okabayashi et al. [4] analysed the medical records of 36 patients who underwent surgical resection of CSGB between 1971 and 2009. Survival after operative management was 37.2% at 1 year, 31% at 2 years and 31% at 3 years.
In the case we present, diagnostic biopsies were performed to inform treatment options. The biopsies sought to determine whether the primary disease was hepatic or gallbladder in origin. Evidence of a primary hepatic malignancy or adenocarcinoma of the gallbladder would have presented wider options for this patient. However, given the poor prognosis of CSGB with extensive metastases, operative management and chemotherapy were not recommended.
Of the 40 cases of CSGB reported in the last 10 years, including the one presented here, the surgical treatment of choice was most often an extended cholecystectomy. This prompts us to surmise that most patients had locally advanced disease at time of diagnosis. Only eight patients underwent a simple cholecystectomy suggesting an early stage carcinosarcoma, and in these cases, the diagnosis of gallbladder malignancy was not suspected preoperatively. Overall, 24 patients underwent an extended cholecystectomy, including between four and seven of whom had adjuvant chemotherapy. In most cases, chemotherapy was not reported to provide significant advantage in terms of morbidity or mortality outcomes. However, in a case with one of the longest survivals reported (alive at 5 years), the patient underwent 3 years of adjuvant chemotherapy with gemcitabine [7] after an extended hepatectomy, portal thrombectomy and hepatoduodenal ligament lymphadenectomy. Four patients underwent palliative resections. Two case reports did not describe treatment. Only one patient, apart from the case we present, was palliated without any surgical intervention. Given the poor prognosis of CSGB, particularly when diagnosed at locally advanced or disseminated stages, we suggest a greater role should be considered for laparoscopic tissue diagnosis before radical surgical intervention. With this approach, unnecessary treatment-related morbidity could be avoided and a greater emphasis be given to the quality of remaining life. The poor prognosis of CSGB, even with surgical intervention, should be acknowledged. This may promote further advances into the role of palliative chemotherapy and other non-surgical interventions in the management of this rare malignancy.
CONFLICT OF INTEREST STATEMENT
There are no conflicts of interest to declare.
FUNDING
There was no funding for this case report.
ETHICS APPROVAL
Ethics approval was not required from the institution for the publication of this case report.
CONSENT
Informed consent was obtained from the patient for the publication of this case report and accompanying images.



