-
PDF
- Split View
-
Views
-
Cite
Cite
Efstathios Pavlidis, Christoforos Kosmidis, Konstantinos Sapalidis, Alexandros Tsakalidis, Dimitrios Giannakidis, Vasileios Rafailidis, Georgios Koimtzis, Isaak Kesisoglou, Small bowel obstruction as a result of an obturator hernia: a rare cause and a challenging diagnosis, Journal of Surgical Case Reports, Volume 2018, Issue 7, July 2018, rjy161, https://doi.org/10.1093/jscr/rjy161
Close - Share Icon Share
Abstract
Obturator hernias are exceedingly rare in surgical routine, constituting 0.073% of all intra-abdominal hernias in the West and 1% in the far East. Commonly known as ‘little old lady’s hernia’, obturator hernias are usually seen in frail, octogenarian multiparous women. This case report discusses an 85-year-old female who had symptoms of acute bowel obstruction; thanks to high degree of clinical suspicion and aided by a computed tomography (CT) of abdomen and pelvis, an incarcerated right obturator hernia was diagnosed preoperatively and treated successfully. Obturator hernia is a rare condition associated with a high rate of morbidity and mortality. CT scan is the most accurate imaging method for pre-operative diagnosis. Early diagnosis and surgical intervention are fundamentals to lead to better outcomes for the patients.
INTRODUCTION
Obturator hernias are exceedingly rare in surgical routine, constituting 0.073% of all intra-abdominal hernias in the West and 1% in the far East [1]. Commonly known as ‘little old lady’s hernia’, obturator hernias are usually seen in frail, octogenarian multiparous women. They are potentially the most lethal of all abdominal wall hernias, notoriously difficult to diagnose in the absence of specific symptoms and signs, and when diagnosed late, frequently necessitating small bowel resection. Even less frequently they are diagnosed preoperatively, with the vast majority being found incidentally at laparotomy for small bowel obstruction.
CASE REPORT
This case report discusses an 85-year-old female who had symptoms of acute bowel obstruction; thanks to high degree of clinical suspicion and aided by a computed tomography (CT) of abdomen and pelvis, an incarcerated right obturator hernia was diagnosed preoperatively and treated successfully.
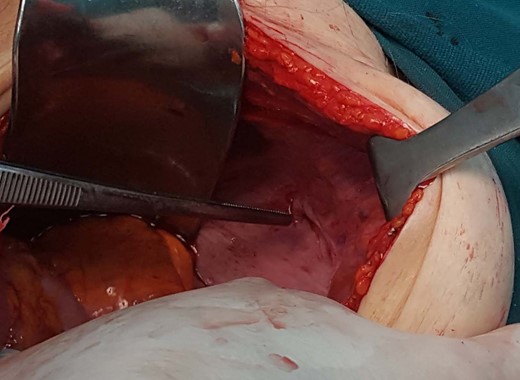
The patient, was admitted to the hospital’s emergency department with a 24-h evolution of diffuse abdominal pain and progressive abdominal distension, associated with persistent vomiting and irradiating pain to the right leg. Patient had a previous history of abdominal surgery including laparoscopic cholecystectomy and repair of umbilical hernia, as well. Physical examination revealed an under-weight female, with distended and tympanitic abdomen, hyperactive bowel sounds with audible rushes associated with vigorous peristalsis, diffuse abdominal pain to deep palpation and no signs of peritoneal irritation or inguino-abdominal hernias. There were neither faeces nor intraluminal mass or blood on the digital rectal examination. Besides, Howship–Romberg sign was negative. The patient maintained her haemodynamic and ventilatory stability. Naso-gastric tube drained ~300 mL of fecaloid fluid. Laboratory exams showed leukocytosis (14 280–70.01% neutrophils) and an increased C-reactive protein level (4.3 mg/L). Upright radiographs demonstrate multiple, short air-fluids levels. Based on the suspicion of an acute bowel obstruction a CT of the abdomen and pelvis was the best applicable solution. The CT scan identified a small intestine segment strangulated through the right obturator foramen and an intestinal distension proximally (Fig. 1). Soon after, the patient underwent an emergent infraumbilical midline laparotomy that confirmed the diagnosis; right obturator hernia with ileal partial wall strangulation (Richter’s type). This was gently released and found to be congested although still viable. Once the bowel loop was released and subjected to warm packs, the colour returned to normal. The obturator hernia defect was roughly 1 × 1 cm2 and this was closed using a single stitch of absorbable polyglactin no. 2 suture (Fig. 2). No other pathology was found. Mass closure of laparotomy wound was with loop polydioxanone (PDS) suture and clips to close the skin. The patient remained stable postoperatively over the course of her hospitalization. She tolerated an oral diet on the second and was discharged on the fourth postoperative day respectively, with an uneventful postoperative recovery.
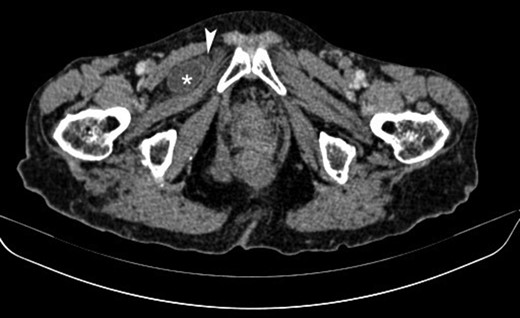
Axial contrast-enhanced CT image showing a small bowel loop (asterisk) appearing herniated and situated superficially to the obturator externus muscle and deep to the pectineus muscle on the right. Note is made of a small fluid collection adjacent to the herniated loop (arrowhead).
DISCUSSION
Obturator hernias usually affect elderly thin women. This is thought to be due to the fact that women have wider pelvis, larger obturator foramen and atrophy or loss of pre-peritoneal fat around the obturator vessels predisposing to hernia formation. Obturator hernia is seen with a rate of 0.4% among bowel obstructions and 0.073–1.0% among hernias [1]. Obturator hernia was first described in 1724 by Ronsil. It occurs with the passing of the hernia sac down from the obturator foramen where the obturator nerve and muscle pass. Chronic obstructive pulmonary diseases, malnutrition, chronic constipation and diseases that cause increased intra-abdominal pressure are among the other predisposing factors. Moreover, obturator hernia is associated with a high mortality rate. This may be attributed to the fact that it is difficult to be diagnosed clinically as signs and symptoms may be non-specific. In fact, most obturator hernias (88%) have been diagnosed when presenting as small bowel obstruction. Patients may also present with a palpable mass in the groin identified when the patient is supine with hip flexed and laterally rotated. Other presentations may include pain on the medial aspect of the thigh on extension, adduction or medial rotation of the hip (Howship–Romberg sign) or loss of adductor reflex (Hannington-Kiff sign) on examination [2]. Given the difficulty in diagnosing obturator hernias, CT scan is the choice of imaging for diagnosis. Surgical intervention is the definitive management of an obturator hernia causing small bowel obstruction; retro-pubic and trans-peritoneal inguinal approach, laparotomy with low midline incision and laparoscopic surgery, preferred more common recently, are among the favourite surgical methods. In cases of emergency admission with small bowel obstruction the standard operation would be a laparotomy with an infraumbilical midline incision, but there may be occasions when laparoscopy could be considered. There have been a few published case series in selected situations suggesting that laparoscopic repair can be used in the acute setting with incarcerated obturator hernias [3]. If the bowel is suspected to be ischaemic on CT a laparotomy is favoured, the advantage being that the site of obstruction can be quickly identified and managed. In our case we used simple sutures, which have been shown to be effective and safe when closing the hernial defect for obturator hernias [2]. Some recent case series have shown that a laparoscopic two-step approach can be taken in patients who have incarcerated hernias requiring bowel resection. One study initially used a laparoscopic bowel resection followed by a totally extraperitoneal mesh repair 9 days later [3]. Another study used a transabdominal pre-peritoneal repair as the second step following initial laparoscopic bowel resection [4].
Due to the aforementioned, obturator hernia is a rare condition associated with a high rate of morbidity and mortality [5, 6]. Its diagnosis is considered a challenge because of its non-specific symptoms and signs and the low rate of occurrence compared to other abdominal hernias. CT scan is the most accurate imaging method for pre-operative diagnosis. There are a limited number of studies with selective criteria describing laparoscopic repair of obturator hernia in the emergency setting. Lower midline infraumbilical laparotomy is a safe and quick method to identify and repair an obturator hernia without complication. A laparotomy additionally allows inspection of the bowel for viability. Early diagnosis and surgical intervention are fundamentals to lead to better outcomes for the patients [7, 8].
CONFLICT OF INTEREST STATEMENT
Authors declare no conflict of interest.



