-
PDF
- Split View
-
Views
-
Cite
Cite
G Rizzo, C Coramusi, G Pietricola, F Sionne, F Castri, D P Pafundi, R Aversa, C Coco, Laparoscopic approach for a presacral myelolipoma resembling a liposarcoma, Journal of Surgical Case Reports, Volume 2018, Issue 7, July 2018, rjy156, https://doi.org/10.1093/jscr/rjy156
Close - Share Icon Share
Abstract
Myelolipomas are rare benign tumors that are commonly found in the adrenal glands. Extra-adrenal locations are rare, and presacral myelolipomas represent the most common extra-adrenal location. The differential diagnosis of malignant presacral neoplasms is very challenging. We present a case of a presacral neoplasm that was completely removed with a laparoscopic approach and diagnosed as a myelolipoma only after pathological examination.
INTRODUCTION
Myelolipomas are rare, small, benign and non-functioning tumors composed of mature adipose tissue and variable amounts of hematopoietic elements. Myelolipomas are commonly found in the adrenal glands, but several extra-adrenal locations have been reported [1, 2]. Myelolipomas are usually asymptomatic and are often discovered incidentally [2]. A certain differential diagnosis with malignant masses is often a clinical problem [3]. If we suspect the possibility of a malignant tumor, an imaging-guided biopsy is contraindicated due to the risk of tumor spread along the biopsy tract [2]. Surgical resection is only indicated when the nature of the tumor is in question or when tumor-related complications occur [4]. In the literature, only two cases of laparoscopic excision of an extra-adrenal myelolipoma are described, one in the presacral area [4, 5].
We report a case of an asymptomatic 72-year-old woman with an incidental diagnosis of a presacral mass of uncertain nature that was defined as myelolipoma only after laparoscopic resection during simultaneous bilateral ovariectomy.
CASE REPORT
An asymptomatic 72-year-old woman with a history of hysterectomy without ovariectomy underwent a pelvic ultra-sound that revealed a cystic formation on the left ovary. Pelvic magnetic resonance (MR) confirmed the diagnosis of a left ovarian cyst and revealed a solid expansive mass in the presacral area that was ~6 cm in diameter, had a lobulated morphology, was strictly adherent to the sacral periosteum, was mainly adipose but exhibited an extremely non-homogeneous signal intensity (Fig. 1). The MR framework did not exclude the diagnosis of a malignant neoplasm such as a liposarcoma. The patient also underwent a contrast-enhanced CT scan that revealed the presence of an elongated formation of mainly adipose density (but with multiple areas of structural non-homogeneity) that was adherent to the presacral fascia (without bone infiltration) and exhibited a modest enhancement; the presence of multiple areas of structural non-homogeneity and modest enhancement precluded the exclusion of a malignant liposarcoma (Fig. 2). The risk that it was a malignant neoplasm contraindicated the execution of a CT-guided biopsy.
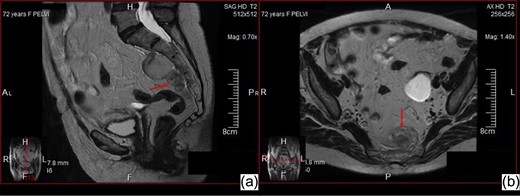
Abdominal MR sagittal (a) and axial (b) images—Solid expansive mass in the presacral area, with lobulated morphology, strictly adherent to the sacral periosteum, with adipose but non-homogeneous signal intensity.
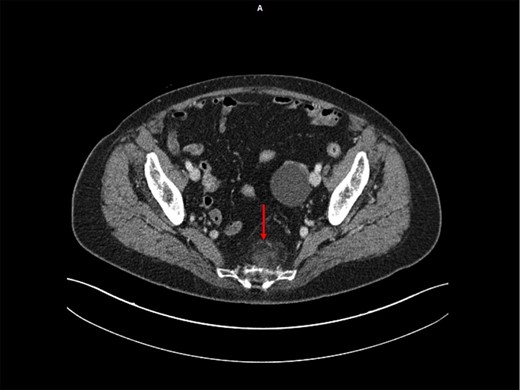
Abdominopelvic CT scan following injection of iodinated contrast agent—Presacral elongated formation of adipose density with multiple areas of structural not-homogeneity, with regular margins, adherent to the presacral fascia (but without bone infiltration) and with a modest enhancement after IV injection.
Considering the need to remove both the ovaries and the presacral mass, we opted for a laparoscopic approach. Upon laparoscopic exploration of abdominal cavity, the cystic formation of the left ovary was confirmed, and a bilateral ovariectomy was performed due to the age of patient. After mobilization of the sigmoid and intra-peritoneal rectum, the pelvic space and the presacral area were exposed to gain access to the lesion that was observed on the MRI and CT. The mass was multilobulated and well-encapsulated. The mass appeared to be easily dissociable from the mesorectal fascia, but it was tenaciously attached to the presacral fascia and strongly suspicious for neoplastic infiltration. An en bloc removal of the neoplasm with clear margins was performed, and the portion of the presacral fascia that was tenaciously adherent to the mass was included in the exeresis. After the removal of the neoplasm, the site of the exeresis appeared to exhibit significant bleeding; therefore, we performed hemostasis by placing hemostatic material (oxidized and regenerated cellulose topical hemostatic dressings).
Pathological examination revealed mature adipose tissue mixed with hematopoietic tissue, which included erythrocytes, myelocytes and megakaryocytes (Fig. 3). There was no evidence of malignancy. These findings were consistent with a presacral myelolipoma.
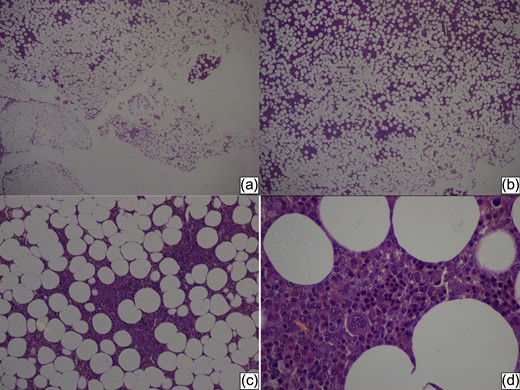
Histopathology of the tumor—Overview (a, b) of the tumor adipose tissue with area of cellular thickening, at the top left (HE stain ×5). At a magnification, HE stain ×20 (c) and HE stain ×40 (d) we can see elements of hematopoiesis: a multinucleated central megakaryocyte, an erythrone, which is the precursor of the erythroid line, and plasma cells with the carriage wheel nuclear chromatin.
DISCUSSION
Myelolipomas are rare, well-encapsulated, benign tumors that contain mature adipose tissue and various combinations of hematopoietic cells [4]. The etiology is unknown. Approximately 50 cases of extra-adrenal myelolipoma are reported in the literature [6]. The extra-adrenal locations include the presacral and perirenal retroperitoneum, mediastinum, stomach, liver, lungs, pelvis, spleen, mesentery and muscle fascia [2].
Myelolipomas are usually asymptomatic and are found incidentally [7]. However, these lesions can become symptomatic due to tumor rupture with secondary bleeding or due to mass effects on adjacent structures [7].
Pathologically, presacral myelolipomas are typically round or oval masses, well-encapsulated and adherent to the sacrum without invasion of the bone or sacral nerve roots. The presence of mature adipose tissue mixed with hematopoietic elements is mandatory for the diagnosis of myelolipoma [8]. Malignant degeneration has never been reported.
Imaging plays an important role in establishing the certain diagnosis of myelolipoma and in excluding the malignant aspects of a presacral mass. Upon CT scan, these lesions usually exhibit some intra-lesional areas and hematopoietic solid tissue islands with variable contrast enhancement [1]. Myelolipomas never invade the adjacent structures. On MRI, the fatty elements exhibit high signal intensities on T1w and T2w sequences, and the hematopoietic tissue islands exhibit lower signal intensities on T1w and T2w with variable contrast enhancement [6]. Differentiating presacral myelolipomas from malignant masses (such as liposarcoma) represents a crucial aspect of patient management; however, a certain diagnosis of a benign mass is not simple to obtain [3]. When a pathological examination (by CT or US-guided fine needle biopsy) is necessary to obtain the correct diagnosis [9]. However, during these procedures, there are risks of malignant spread along the biopsy tract, bleeding and sampling error [2].
Actually, laparoscopic approaches for abdominal diseases are considered valid alternatives to open approaches, especially if surgery is necessary for a diagnostic purpose [10].
In the literature, only two cases of laparoscopic excision of an extra-adrenal myelolipoma are described [4, 5], one in the presacral region [4]. The presacral myelolipoma was laparoscopically managed during a sigmoid resection for diverticular disease. During this procedure, subtotal excision of the mass and intra-operative pathological examination were performed (the latter confirmed the benign nature of the mass). Given the non-malignant frozen pathology results, no further attempts were made for complete removal [4].
In our case, surgery was necessary to establish the real nature of the presacral mass because the imaging was not able to exclude a malignant liposarcoma. Moreover, intra-operatively, the characteristics of the lesion were similar to those of a malignant neoplasm. According to these findings, we performed complete removal of the neoplasm. The mini-invasive approach was able to completely remove the neoplasm and thus could represent a valid method for establishing a certain diagnosis.
Conflict of Interest statement
The authors declare that they have no conflict of interest.



