-
PDF
- Split View
-
Views
-
Cite
Cite
Young Lee, Gregory Zielinski, Jasmine Bhinder, Sandeep Sirsi, Armand Asarian, A rare case of percutaneous endoscopic gastrostomy causing a small bowel obstruction and subsequent bowel erosion, Journal of Surgical Case Reports, Volume 2018, Issue 7, July 2018, rjy160, https://doi.org/10.1093/jscr/rjy160
Close - Share Icon Share
Abstract
Gastrostomy tubes can be used to provide long-term nutrition and feeding when oral intake is not adequate. A rare but serious complication includes iatrogenic small bowel injury. The incidence of this is infrequent due to its position of the small bowel beneath the omentum, however, injury leading to obstruction and volvulus has been previously described in the literature. We present an unusual case of gastrostomy tube transection into omental fat causing a kink in the small bowel allowing for a transition point of obstruction and subsequent erosion of the gastrostomy tube into the small bowel.
INTRODUCTION
Gastrostomy tubes can be used to provide long-term nutrition and feeding when oral intake is not adequate. They can be placed surgically or endoscopically and the complications with either method are similar [1]. Complications range from minor infections and bleeding to severe necrotizing fasciitis and gastric perforation. Other rare but serious complications include iatrogenic injury to surrounding organs such as the spleen, liver and bowel [1]. The incidence of small bowel injury is infrequent due to its position beneath the omentum; however, injury leading to obstruction and volvulus has been described in the literature [2, 3].
CASE REPORT
A critically ill 74-year-old female underwent tracheostomy and subsequent percutaneous endoscopic gastrostomy (PEG) tube placement. On the following day, after starting feeds through the PEG tube, the patient developed abdominal distention. An abdominal X-ray showed possible concern for a small bowel obstruction (SBO). A computed tomography (CT) scan further confirmed dilated small bowel loops proximally with distal collapse and transition point near the gastrostomy tube site. On sagittal view, the small bowel appeared entrapped between the abdominal wall and the stomach (Fig. 1). All feeds were stopped and the PEG tube was placed on gravity drainage to decompress the stomach and small bowel.
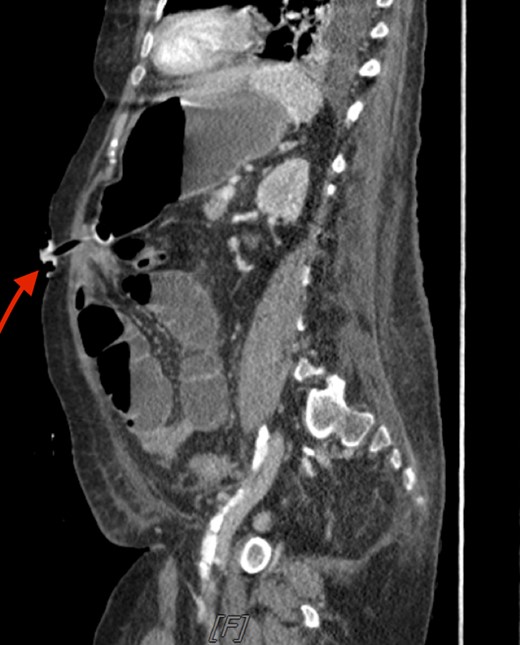
Sagittal CT scan of the abdomen. The arrow is pointing to the small bowel entrapped between the abdominal wall and stomach.
Patient failed to improve with nonoperative management and the surgery team was consulted for bowel obstruction seen on CT scan. Physical exam revealed increased abdominal distention despite decompression and the abdomen was diffusely peritonitic. Subsequently, a diagnostic laparoscopy with possible laparotomy was scheduled. After induction of anesthesia, a laparoscope was inserted into the abdominal cavity. Upon immediate inspection, enteric contents were encountered and the small bowel was seen adherent between the gastric lumen and the anterior abdominal wall. The PEG tube had transected into omental fat causing a kink in the small bowel allowing for a transition point of obstruction and subsequent erosion of the gastrostomy tube into the small bowel. At this time, a midline incision for laparotomy was made to resect the eroded small bowel and an side-to-side enteroenterostomy was performed. The abdominal cavity was thoroughly irrigated and no other intra-abdominal abnormalities were noted. Patient was then transferred to the postanesthesia care unit in stable condition for recovery.
DISCUSSION
PEG tube insertion is typically considered a safe procedure, however, complications can occur and are well documented. Minor complications include wound infections, tube leakage to abdominal cavity, stoma leakage, inadvertent PEG removal, tube blockage, pneumoperitoneum, gastric outlet obstruction and peritonitis. Some of the major documented complications include aspiration pneumonia, hemorrhage, buried bumper syndrome, perforation of bowel, necrotizing, metastatic seeding [1].
Our patient presented with an interesting and rare complication. After the PEG tube was placed, the patient had a normal postoperative presentation. The abdomen was soft, nontender and nondistended. Upon feeds being started through the PEG tube, the patient presented with symptoms of a bowel obstruction. The patient’s abdomen became very distended and she started experiencing vomiting. The tube feeds were held, the PEG tube placed on gravity drainage with immediate bilious fluid return, and the patient was monitored. However, the patient’s abdominal distention persisted and ultimately, the abdomen then became peritonitic on physical exam. At this time, it was decided that surgical intervention was necessary to explore and diagnose the abdominal pathology given that a recent intervention caused the obstruction and peritonitis.
CONFLICT OF INTEREST STATEMENT
None declared.



