-
PDF
- Split View
-
Views
-
Cite
Cite
Ryan D Konik, Ronald A Rhodes, Complete small bowel obstruction without intussusception due to a submucosal lipoma, Journal of Surgical Case Reports, Volume 2018, Issue 7, July 2018, rjy155, https://doi.org/10.1093/jscr/rjy155
Close - Share Icon Share
Abstract
Submucosal lipomas of the small bowel are rare, often asymptomatic, benign tumors. Large lesions may present with acute symptoms such as a bowel obstruction from an intussusception or acute hemorrhage. Acute findings such as these require operative intervention. In this case, we present a 53-year-old female with a complete small bowel obstruction secondary to a submucosal lipoma without signs of an intussusception.
INTRODUCTION
Lipomas of the small bowel are rare, benign mesenchymal tumors. They can appear in any area of the gastrointestinal tract with the most common location being the colon, followed by the small bowel, and occasionally in the foregut [1]. A small lesion is frequently asymptomatic, but a lesion >2 cm can cause acute symptoms, such as intussusception or hemorrhage [2]. Operative intervention is required in the presence of peritonitis, perforation, massive hemorrhage, intussusception or complete obstruction. There have been reports of large small bowel lipomas causing obstruction from an intussusception, but none reporting small lesions causing complete obstruction without intussusception. We report a case of complete small bowel obstruction without intussusception secondary to a small submucosal lipoma of the distal jejunum.
CASE REPORT
A 53-year-old female presented with abdominal pain, distension, nausea and vomiting for 1-day duration. Her past medical history was consistent with hypothyroidism and alcohol abuse with a reported use of one pint of hard liquor per day for several years. In addition, she reported chronic issues with constipation and nausea requiring as needed use of anti-diarrheal and anti-emetic medications. She reported no surgical history. Physical examination demonstrated a soft, distended abdomen with diffuse tenderness and no peritoneal signs. A non-contrasted computer tomography scan of the abdomen and pelvis demonstrated dilated loops of small bowel extending from the proximal ileum to the distal duodenum with a small quantity of ascites. Findings were consistent with an incomplete, distal small bowel obstruction. The patient was admitted, and a trial of conservative management was attempted. She was made nil per os, fluid resuscitated and had a nasogastric tube placed for proximal decompression.
She showed minimal signs of improvement after 24 h. A small bowel follow through with Gastrografin was ordered. This study identified a complete obstruction in the mid-segments of the small bowel corresponding to the distal jejunum, proximal ileum (Fig. 1). An exploratory laparotomy was performed on post-admission Day 2 due to the findings of a complete obstruction. During the operation, the small bowel appeared hyperemic and dilated. The small bowel was inspected from the ligament of Treitz to an area of transition. At this point, the distal small bowel was decompressed, and an intraluminal mass was palpated. A small bowel resection with a side-to-side anastomosis was performed. The gross specimen was opened and contained an intraluminal mass with the characteristics of a lipoma (Fig. 2). Pathologic evaluation of the specimen showed a 1.5 × 1 × 1 cm3 submucosal lipoma with a small area of overlying ulceration and no evidence of malignancy (Fig. 3). The rest of her hospital course was complicated by a fascial dehiscence requiring retention suture placement. She was discharged on post-operative Day 18.
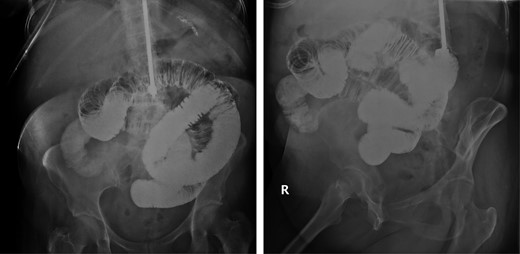
Small bowel follow-through with gastrograffin showing completed obstruction after 8 h in the mid-right lower mesogastric region.

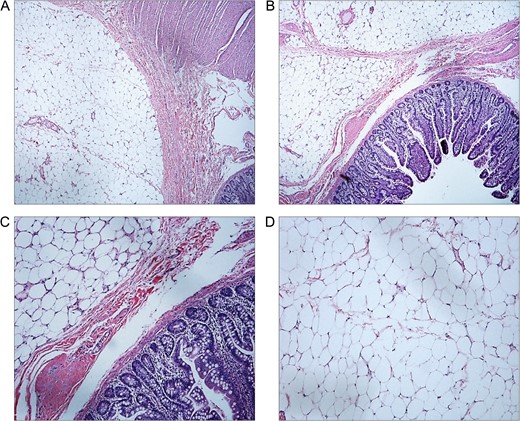
Histology of surgical specimen. (A) and (B) Submucosal lipoma with normal jejunum (H&E stain, ×40 magnification). (C) Submucosal lipoma with normal jejunum (H&E stain, ×100 magnification). (D) Lipoma (H&E stain, ×100 magnification).
DISCUSSION
Lipomas of the gastrointestinal tract are rare, benign tumors of mesenchymal origin. Tumors of the small bowel account for 1–2% of all gastrointestinal tumors with 30% of those being benign [3]. The majority of lipomas occur in the colon, but they can be present throughout the entire gastrointestinal tract. About 20–25% of gastrointestinal lipomas present in the small intestine, with the ileum being the most common location followed by the jejunum [1, 2, 4]. Gastrointestinal lipomas are rarely symptomatic. Lesions greater than 2 cm in diameter may cause non-specific symptoms such as abdominal pain, diarrhea and hematochezia [2]. Acute manifestations, such as partial or complete obstructions, are infrequent occurrences. Bowel obstructions secondary to intestinal lipomas result from intussusception in the majority of documented case reports [1–3]. This is the first reported case of a small bowel lipoma causing a complete obstruction without evidence of an intussusception. In addition, the submucosal lipoma occurred in the distal jejunum, which is a rare location occurrence for such a benign mass.
Preoperative diagnosis of lipomas can be accomplished by imaging or endoscopic modalities. Computed tomography (CT) scans of the abdomen may reveal a mass with a uniform and fatty tissue density consistent with a lipoma. Small intestinal series demonstrating a radiolucency and a ‘squeeze sign’ indicating an altered configuration during peristalsis are characteristic findings suggestive of a lipoma [5]. Endoscopic methods, include capsule endoscopy and digital balloon endoscopy, are useful for the diagnosis of lipomas within the small intestine. Colonoscopy can diagnosis lipomas within the colon. The ‘cushion sign’, the ‘tenting effect’ and the ‘naked fat sign’ are characteristic findings associated with lipomas of the colon [1, 5]. CT of the abdomen and pelvis and a small intestinal series were incorporated in the management of the presented case. However, these imaging studies only identified findings consistent with a complete small bowel obstruction without a noticeable mass.
Operative intervention is often required for complete small bowel obstructions. Partial obstructions can be managed conservatively with nil per os, fluid resuscitation, and nasogastric tube decompression; however, if there are no signs of improvement, operative intervention may be indicated. Exploratory laparotomy and diagnostic laparoscopy are surgical options that are determined by patient characteristics and surgeon preference. This case represents a rare occurrence of a complete small bowel obstruction secondary to a submucosal lipoma and highlights the associated diagnostic and treatment challenges.
CONFLICT OF INTEREST STATEMENT
None declared.



