-
PDF
- Split View
-
Views
-
Cite
Cite
Sachin Teelucksingh, Leela Krishna Teja Boppana, Sanjeeva Goli, Vijay Naraynsingh, Gallstone ileus 1 year after cholecystectomy, Journal of Surgical Case Reports, Volume 2018, Issue 7, July 2018, rjy153, https://doi.org/10.1093/jscr/rjy153
Close - Share Icon Share
Abstract
Post-cholecystectomy gallstone ileus (GSI) is very rare with only 16 cases reported in the literature. This condition poses diagnostic challenges both because of its rarity and since the gallbladder had been previously removed. A high index of suspicion is needed for diagnosis. We report a case of a 37-year-old female who presented with GSI 12 months post-cholecystectomy.
INTRODUCTION
Gallstone ileus (GSI) is a well-recognized albeit relatively rare cause of bowel obstruction due to impaction of a gallstone in the gut usually the ileum; it accounts for 1–4% of all cases of bowel obstruction (1). It is quite rare however, for GSI to present long after cholecystectomy and only 16 such cases have been reported (2). We here contribute a further case, one who developed GSI 1 year post-cholecystectomy.
CASE REPORT
A 37-year-old female presented to the Emergency Department with sudden onset of colicky abdominal pain, increasing in frequency and severity over the preceding 24 h. Prior to the onset of pain, she had an episode of profuse, bilious vomiting followed by a further 5 bouts during the course of the day. She also had 2 bowel movements within 2 h of the onset of abdominal pain but no flatus or faeces thereafter. Two weeks earlier, she had abdominal discomfort while passing stool and a sense of persistent bloating. Twelve months earlier, she had an open cholecystectomy for severe cholecystitis complicated by empyema.
Examination revealed a young woman who was afebrile and anicteric. Abdominal examination revealed minimal distension, generalized mild tenderness, but no rebound or guarding.
Laboratory investigations (biochemical profile and urinalysis) were all within normal limits. Abdominal CT showed pneumobilia and a 2 cm intraluminal density in the distal ileum with resultant small bowel obstruction (Figs 1 and 2). She underwent emergency laparotomy and enterolithotomy followed by a smooth postoperative course (Figs 3 and 4). The CT scan taken elsewhere and just prior to the emergency cholecystecomy 12 months earlier was reviewed; this demonstrated a markedly distended gallbladder with irregular wall thickening and severe pericholecystic fat stranding consistent with a gallbladder empyema measuring 16 cm × 9.0 cm. There were also multiple gallstones with the largest two measuring 2 cm at the neck of the gallbladder and the other, 2.0 cm in diameter at the fundus of the gallbladder, respectively. There was a narrower, septum-like area between the neck and grossly distended empyema (Fig. 5)
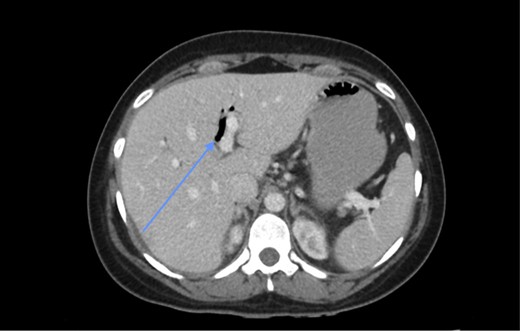
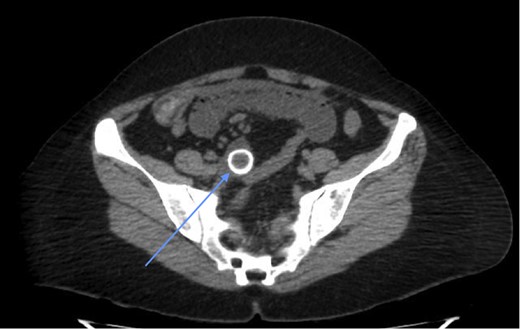
CT scan showing a rim-calcified gallstone, causing ileal obstruction.


Gallstone after delivery by enterolithotomy. The gallstone measured 2 cm in diameter.

CT scan prior to cholecystectomy, 12 months earlier, showing calcified gallstones within gallbladder empyema and a septum-like narrowing (arrow) between the neck and the grossly distended empyema.
DISCUSSION
GSI develops only in 0.3–0.5% of patients with cholelithiasis (3). The typical patient who presents with GSI has a history of acute or chronic cholecystitis at which time the gallbladder adheres to the duodenum leading to the formation of a fistula. The vast majority (96.5%) are associated with a cholecystoduodenal fistula (1). Subtotal cholecystectomies are done when there is severe inflammation of the gallbladder and this can be a safe option to avoid dissection of Calot’s triangle (4). However, after such a procedure it must be ensured that the remnant is free of gallstones, as there have been complications such as choledocholithiasis, persistent biliary fistula, gallstone pancreatitis and acute cholecystitis related to such a procedure (5). We believe that, in our case, the gallbladder was transected between the neck and the grossly distended empyema, leaving a large gallstone at the neck (Fig. 5). Subsequent stump cholecystitis with fistula formation would have delivered the 2 cm gallstone into the gut causing GSI, since the calcified stone at the gallbladder neck 1 year before is very similar to the one obstructing the ileum.
Only 16 cases of GSI post-cholecystectomy have been recorded (6). In order to make this diagnosis, one needs to have a high index of clinical suspicion. The history and physical examination are non-specific and laboratory investigations are not very helpful. Radiological studies are most diagnostic using Rigler’s triad, which is pathognomic. The triad includes pneumobilia, an ectopic stone and signs of bowel obstruction. In making the diagnosis, abdominal CT is best, having a sensitivity, specificity and accuracy of 93%, 100% and 99%, respectively, and is considered the gold standard (7).
There is a remarkable report of a very unusual case in which Zens et al. recorded a 91-year-old female who was purported to have had GSI 30 years post-cholecystectomy (8). However, it is noteworthy that this patient had a large duodenal diverticulum, which could have extruded an enterolith that caused the bowel obstruction; this likelihood is also supported by the absence of pneumobilia.
The treatment of GSI varies. The choice of procedure depends on the surgeon, patient demographics and comorbidities. Treatment in a patient who presents post-cholecystectomy is simple enterolithotomy. Reissner et al. in a review of 1001 patients, state that the one stage procedure (enterolithotomy, cholecystectomy and fistula closure) has a mortality of 16.9% as opposed to 11.7% for enterolithotomy. There has been a recurrence rate of 5% of GSI after the one stage procedure (9). Few studies have reported on the two-stage procedure (enterolithotomy with cholecystectomy performed later) (2). Ravikumar et al. concluded that enterolithotomy is the ‘best option for most patients’ while the one stage procedure may be considered for ‘low-risk patients’.
CONCLUSION
Post-cholecystectomy GSI is quite rare but clinicians should be aware of its existence since the diagnosis requires a high index of suspicion, which can be confirmed with an abdominal CT. The treatment is surgical; simple enterolithotomy is the treatment of choice for most cases.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
There was no source of funding for this report.
CONSENT
Informed Consent was provided by the patient.



