-
PDF
- Split View
-
Views
-
Cite
Cite
Jumana A Hussain, Hussain Al Zamel, Bhaimtyaz Nawaz, Angiolymphoid hyperplasia with eosinophilia (epithelioid hemangioma) of the external auditory canal, an unusual presentation in an adult female: a case report, Journal of Surgical Case Reports, Volume 2018, Issue 7, July 2018, rjy145, https://doi.org/10.1093/jscr/rjy145
Close - Share Icon Share
Abstract
Introduction: Angiolymphoid hyperplasia with eosinophilia (ALHE) is a rare entity that usually occurs as 0.5–3 cm, pink-to-brown nodules on the skin surface and subcutaneous tissues of the head and neck (Al-Muharraqi MA, Faqi MK, Uddin F, Ladak K, Darwish A. Angiolymphoid hyperplasia with eosinophilia (epithelioid hemangioma) of the face: an unusual presentation. Int J Surg Case Rep 2011;2:258–60.; Suzuki H, Hatamochi A, Horie M, Suzuki T, Yamazaki S. A case of angiolymphoid hyperplasia with eosinophilia (ALHE) of the upper lip. J Dermatol 2005; 32:991–5.). Case presentation: A 29-year-old woman presented to our ENT (ear-nose-throat) clinic with multiple, small reddish to pinkish nodules of approximately 1 × 2 cm2 in dimension. A biopsy from the surface of the left external auditory canal skin, where she had severe itching, showed features consistent with Angiolymphoid hyperplasia with eosinophilia ALHE. Discussion: Whether angiolymphoid hyperplasia with an eosinophilia etiology is a neoplastic or atopic hypersensitivity reaction (unusual reactive process) is controversial. The definitive treatment is surgical excision and follow-up (Al-Muharraqi MA, Faqi MK, Uddin F, Ladak K, Darwish A Angiolymphoid hyperplasia with eosinophilia (epithelioid hemangioma) of the face: An unusual presentation. Int J Surg Case Rep 2011;2:258–60.; Barnes L, editor. Surgical Pathology of the Head and Neck. 3rd edn. New York: Marcel Decker; 2001.). Conclusion: Although ALHE of <3 cm has been rarely reported in the literature, it should be considered in the differential diagnosis of large subcutaneous tumors of the head and neck.
Introduction
Angiolymphoid hyperplasia with eosinophilia (ALHE) (epithelioid hemangioma, inflammatory angiomatous nodule, atypical granuloma, pseudopyogenic granuloma and histiocytoid hemangioma) is an uncommon, benign, reactive vasoproliferative disease, presenting with painless, vascular nodules in the dermal and subcutaneous tissues of the head and neck, particularly around the ear [1]. ALHE has also been reported in the scalp, lip, tongue, orbits and conjunctiva [2]. Although it is usually superficial in nature, some authors have reported muscular and bony involvement [3]. ALHE is somewhat more common in females, but a male predominance has been reported in selected Asian studies. It presents most commonly in patients aged 20–50 years, with a mean age at onset of 30–33 years [4]. This condition is uncommon and is even rarer in elderly patients and non-Asian pediatric populations. ALHE can persist for years, but serious complications (e.g. malignant transformation) do not occur and have never been reported. It is often characterized by a distinctive infiltrate composed of lymphocytes, eosinophils and plasma cells. The condition is confirmed by the histopathological presence of abnormally proliferating, plump endothelial cells often near muscular arteries [4]. ALHE lesions are typically small, pruritic and erythromatous nodules with a diameter ranging from 0.5 to 3 cm, with larger presentations being a relatively rare manifestation. We report an unusual presentation in size and appearance of ALHE in the skin of the external auditory canal of an adult female (Fig. 1).

Showing reddish to pinkish nodular lesion at outer part of external auditory canal of left ear.
The work has been reported in line with the SCARE criteria [5].
CASE PRESENTATION
An otherwise fit and healthy 29-year-old woman presented to our ENT clinic with multiple small reddish to pinkish nodules of ~1 × 2 cm2 in dimension. She had severe itching on the outer part of the left external auditory canal skin. It had slowly enlarged over the last few months. No obvious cutaneous ulceration, crusting and discoloration, which are commonly associated with ALHE, were observed. The lesions were non-tender and fixed, with a smooth surface possessing a solid consistency when palpated (Fig. 1). No regional lymphadenopathy was observed. Routine blood counts were normal. An incisional biopsy was obtained, which showed ALHE. Local treatment with steroid cream and triamcinolone injection was used but without any success. Although the itching sensation was reduced, the lesions had not reduced in size in ~6 months’ follow-up. Thus, the lesions were fully excised under general anesthesia.
Postoperative recovery was excellent, and the patient was discharged on the second postoperative day. Histological examination revealed proliferation of small blood vessels lined with plump endothelial cells and surrounded by a lymphoid infiltrate with formation of germinal centers. Large numbers of eosinophils were observed (Fig. 2). A diagnosis of ALHE was made. No recurrence was found after a follow-up period of 9 months (Fig. 3).

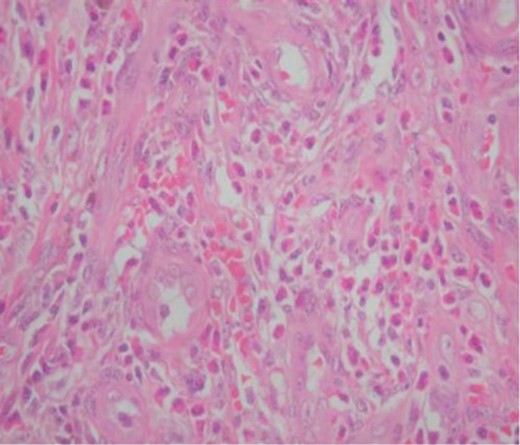
Histopathological picture of the lesion showing plump endothelial cells and surrounded by a lymphoid infiltrate with formation of germinal centers. Large numbers of eosinophils are also seen.
DISCUSSION AND REVIEW OF LITERATURE
Many theories exist to explain the etiology of ALHE. The main contention remains controversial as to whether it is a neoplastic or atopic hypersensitivity reaction (unusual reactive process), with the latter receiving more support [6]. Several reports also indicate the possibility that ALHE may be secondary to infection or trauma [6]. However, the exact relationship of these lesions to each other, including Kimura disease, which represents an allergic or autoimmune response, remains incompletely understood. First described by Wells and Whimster [7], ALHE is a disfiguring lesion characterized by isolated or small numbers of pinkish to reddish-brown papules, frequently in the head and neck region. Although the diameters of the lesions in ALHE have been reported in dated literature to range from 1 to 10 cm, many reported presentations were within 0.5–3 cm in diameter. Larger lesions, falling into the upper end of the spectrum, are relatively rare and have not been reported in the last 30 years. The clear demarcation, insidious growth, and submucosal limitations of the lesion indicated a benign neoplasia. Hence, the differential diagnosis was primarily a mesenchymal tumor of the vessels, nerves, or muscles in the head and neck, namely, neurilemmoma, leiomyoma, hemangioma and fibrosarcoma [8]. Surgical excision is the reported to be the most effective treatment for ALHE. Yet, treatment failure rates as high as 41% are reported for this mode of therapy. Laser approaches are less successful in the management of ALHE, with pulsed-dye laser having the lowest reported failure rate at 50%, followed by carbon dioxide laser at 55% [9]. ALHE can persist for years, but serious complications do not occur. A few cases of nephropathy have been reported in patients with ALHE; however, the association is not strong. This is in contrast to the related entity, Kimura disease, for which the association with nephrotic syndrome is strong. Of note, although, coexistence of Kimura disease and ALHE in the same patient, along with minimal-change glomerulopathy, has been reported [10].
Despite a 33% recurrence rate, our patient had a successful recovery with no recurrence in her 9-month follow-up.
ALHE exceeding 3 cm in diameter has been rarely reported. However, on the basis of our case report, it should be a viable differential diagnosis when large subcutaneous tumors of the head and neck are encountered.
CONCLUSION
ALHE exceeding 3 cm in diameter has been rarely reported. However, on the basis of our case report, it should be a viable differential diagnosis when large subcutaneous tumors of the head and neck are encountered.
CONFLICT OF INTEREST STATEMENT
None of the authors has any conflict of interest to declare.
FUNDING
None.
ETHICAL APPROVAL
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available and can be reproduced whenever needed.
All the procedures performed in the study involving the human participant were in accordance with the ethical standards of the institution.
REFERENCES
- biopsy
- dermatology
- eosinophilia
- adult
- epithelioid hemangioma of skin
- differential diagnosis
- ear
- external auditory canal
- follow-up
- angiolymphoid hyperplasia
- immediate hypersensitivity
- surgical pathology
- pharynx
- lip
- neoplasms
- nose
- pruritus
- skin
- head and neck
- subcutaneous tissue
- excision
- causality
- histiocytoid hemangioma



