-
PDF
- Split View
-
Views
-
Cite
Cite
Nozomi Kikuchi, Yasuyuki Miyakura, Jun Takahashi, Noriya Takayama, Sawako Tamaki, Hideki Ishikawa, Nao Kakizawa, Fumi Hasegawa, Rina Kikugawa, Shingo Tsujinaka, Alan Kawarai Lefor, Toshiki Rikiyama, Intussusception secondary to descending colon lipoma presenting with simultaneous acute appendicitis, Journal of Surgical Case Reports, Volume 2018, Issue 7, July 2018, rjy152, https://doi.org/10.1093/jscr/rjy152
Close - Share Icon Share
Abstract
We report a patient with a descending colon lipoma presenting with hematochezia who developed intussusception, which was simultaneously accompanied by acute appendicitis. A 43-year-old man presented with hematochezia. Colonoscopy revealed a submucosal tumor with a reddish surface in the descending colon. A solid mass with fat density value measuring 5 cm in diameter was observed in the descending colon on CT. While awaiting elective resection, the patient developed lower abdominal pain. CT demonstrated antegrade colo-colonic intussusception in the descending colon. Simultaneously, the appendix was inflamed with a high density intraluminal lesion suspected to be a fecalith. The diagnosis of simultaneous intussusception and acute appendicitis was made. Appendectomy and partial resection of the descending colon was performed. Histopathological examination was consistent with descending colon lipoma and acute appendicitis. The mechanism for developing hematochezia and the risk for development of colo-colonic intussusception due to large colon lipoma and acute appendicitis were highlighted.
INTRODUCTION
Colon lipomas are rare benign lesions representing ~1.8% of all benign colon lesions [1]. These lesions are typically asymptomatic and found incidentally during colonoscopy. Lipomas range in size from millimeters to centimeters in diameter, but symptoms usually occur only when their diameter exceeds 2 cm [2]. In extremely rare cases, these lesions may cause hemorrhage, luminal obstruction or intussusception, which result in acute abdominal pain [3]. On the other hand, acute appendicitis usually presents with periumbilical pain migrating to the right lower quadrant, and is the most common abdominal surgical emergency. We report a patient with a descending colon lipoma who presented with hematochezia, and subsequently developed intussusception with simultaneous acute appendicitis.
CASE REPORT
A 43-year-old man presented to the emergency department with the sudden onset of massive hematochezia. Rectal examination revealed hematochezia, but was negative for hemorrhoids. Laboratory findings were normal except for mild anemia. The patient was admitted for further examination. A submucosal tumor with a reddish surface, measuring 5 cm in diameter, without active bleeding was found on colonoscopy in the descending colon (Fig. 1a). The mucosa surrounding the tumor, especially on the contralateral wall, had mucosal hematoma (Fig. 1b). Biopsy specimens taken from the tumor exhibited only inflammatory tissue. Contrast-enhanced computed tomography (CT) demonstrated a solid mass with fat density of 5 cm in diameter in the descending colon (Fig. 2). The possibility of re-bleeding and malignancy could not be eliminated, and laparoscopic left hemicolectomy was planned.
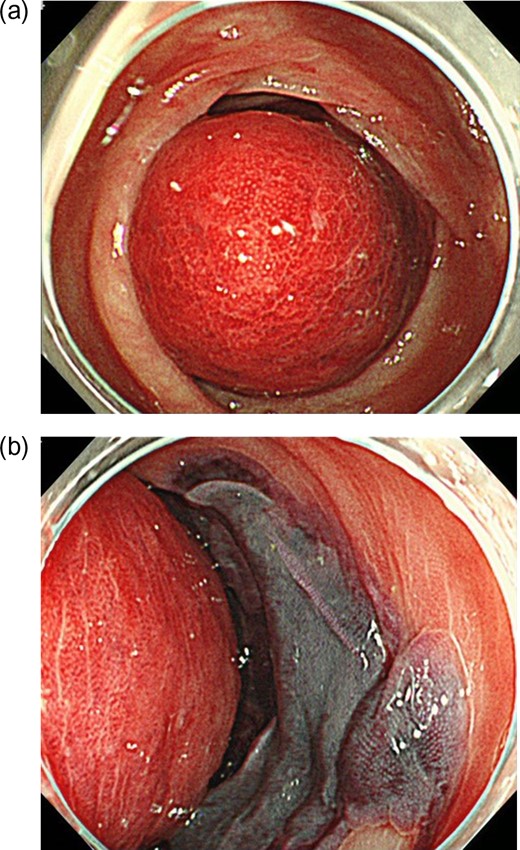
Findings at colonoscopy: (a) A submucosal tumor with a reddish surface and no active bleeding measuring 5 cm in diameter was observed in the descending colon. (b) The mucosa surrounding the submucosal tumor, especially on the opposite side, had mucosal hematoma formation.

CT findings at the time of diagnosis: contrast-enhanced CT of the abdomen at the time of diagnosis revealed a solid mass measuring 5 cm in diameter with fat density in the descending colon (white arrow).
While awaiting surgery, the patient developed sudden-onset lower abdominal pain and was readmitted. On physical examination, the abdomen was distended with right lower quadrant tenderness to palpation and rebound tenderness. Laboratory data revealed elevation of the white blood cell count to 18 000/mm3 and a serum C-reactive protein level of 5.8. Antegrade colo-colonic intussusception was observed on CT with the lipoma of the descending colon as the lead point (Fig. 3a, b). The appendix was acutely inflamed, and calcification was seen in the appendix with inflammatory changes in surrounding tissues (Fig. 3b).

CT findings at the time of readmission: CT of the abdomen at readmission (a: axial view, b: coronal view) demonstrated antegrade colo-colonic intussusception with the lipoma in the descending colon as the lead point (white arrow). The appendix was also found to be swollen with a high density mass suspected to be a fecalith in the lumen, with inflammation in surrounding tissues (b, black arrow).
The diagnosis of simultaneous intussusception and acute appendicitis was made. Appendectomy and partial resection of the descending colon were performed. The surgical specimen revealed a lipoma covered by normal mucosa with bright yellow texture on the cut surface (Fig. 4a). This lipoma measured 42 × 35 mm2 in size, and was composed of mature adipose tissue and covered by normal mucosa, microscopically. The feature of appendiceal lesion was consistent with that of acute gangrenous appendicitis (Fig. 4b). The postoperative course was uneventful.
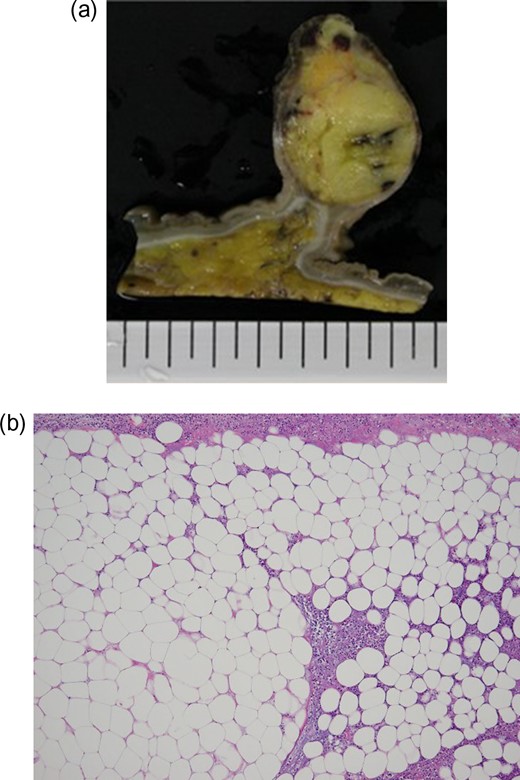
Surgical specimen and histopathological examination: (a) Macroscopically, the surgical specimen revealed a lipoma covered by normal colonic mucosa with well-demarcated, bright yellow texture. (b) Histopathological examination indicated mature adipose tissue (HE ×400).
DISCUSSION
This report describes a patient with a large lipoma of the descending colon who presented with hematochezia caused by a submucosal tumor with hematoma in the surrounding mucosa, particularly on the opposite side of the submucosal tumor. Intussusception incidentally developed while waiting for elective surgery. The symptoms at that time were consistent with acute appendicitis. The occurrence of hematochezia and the risk of developing colo-colonic intussusception due to a large colon lipoma, incidentally accompanied by acute appendicitis, were highlighted in this patient.
Endoscopically, lipomas are generally yellowish polyps with a pedicle or large base, covered by smooth mucosa. Three endoscopic signs may help with the diagnosis: the ‘tenting sign’ (grasping the overlying mucosa), ‘cushion sign’ (flattening and restoration of the shape of the lipoma) and the ‘naked fat sign’ (extrusion of fat after biopsy of the colonic mucosa) [4, 5]. Small lesions are found incidentally, and they are generally both diagnosed and treated endoscopically. In the present patient, the descending colon lipoma was a large submucosal tumor with a reddish surface on endoscopy. The surrounding colon mucosa, especially on the contralateral wall, exhibited hematoma in the mucosa. Mechanical factors due to tumor movement in the lumen may have contributed to hematoma formation and the subsequent hematochezia in this patient. These rare endoscopic findings provide a clue to the mechanism of hematochezia due to large colon lipoma.
It has been suggested that resection should be performed for the following indications: (1) lipoma with a diameter of >4 cm, with a sessile appearance or limited pedicle; (2) unclear preoperative diagnosis; (3) lesions with significant symptoms, especially in the presence of intussusception; (4) involvement of the muscularis or serosa; or (5) if the lesion cannot be resected completely by colonoscopy [2]. In the present patient, laparoscopic resection of this >4 cm submucosal tumor that presented with massive hematochezia was planned. Acute appendicitis accompanying intussusception developed while awaiting surgery and emergent open resection was performed. Over the past 20 years, laparoscopic resection has been widely used, with a significantly shorter length of stay than after open surgery [6]. Laparoscopic resection is considered to be the standard treatment for patients with colonic lipomas.
Acute appendicitis is the most common reason for emergency abdominal surgery in adults. The history and physical findings, especially periumbilical pain that migrates to the right lower quadrant, helps to establish the diagnosis of acute appendicitis. Acute appendicitis simultaneously accompanying intussusception is extremely rare; only one similar case has been reported [7]. In the present patient, the symptoms, physical examination and laboratory findings were consistent with acute appendicitis. The appendix was enlarged with wall thickening on CT, and a high density mass suspected to be a fecalith was observed in the appendiceal lumen, consistent with the findings for acute appendicitis. Simultaneous intussusception of the lipoma in the descending colon was incidentally noted on the CT. The relationship between the occurrence of intussusception and appendicitis is unknown. But increased intraluminal pressure of the colon is considered as one of the cause of acute appendicitis. Intussusception of the descending colon lipoma may lead to colonic obstruction, increased intraluminal pressure and acute appendicitis.
CONCLUSION
Large lipomas of the colon presenting with hematochezia may lead to the development of intussusception. Early resection is recommended after establishing the diagnosis. Physicians should pay attention to the possibility for development of accompanying abdominal conditions while waiting for elective surgery.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest or financial ties to disclose.



