-
PDF
- Split View
-
Views
-
Cite
Cite
Berta Barbosa, Catarina Morais, Sílvia Neves, António Canha, Paulo Soares, Jorge Daniel, Donzilia Sousa Silva, José Davide, Solitary fibrous tumor of the liver. Report of three cases of a very rare tumor, Journal of Surgical Case Reports, Volume 2018, Issue 7, July 2018, rjy150, https://doi.org/10.1093/jscr/rjy150
Close - Share Icon Share
Abstract
Solitary fibrous tumors (SFT) can originate in any site of the body. Hepatic location is extremely rare.
We present three cases corresponding to women of 26, 40 and 78 years old, with the diagnose of a liver tumor, compatible with SFT, discovered on abdominal CT, who were submitted to right, left and atypical hepatectomy, respectively. The first patient has undergone multiple interventions for excision of metastatic lesions, and is stable with trabectedin; the second patient is asymptomatic with no evidence of recurrence; the third patient had recurrence of the disease after 16 months and passed away 32 months after diagnosis.
Hepatic malignant SFT is very rare, although should be consider in the differential diagnosis of a single large hepatic tumor. Definitive diagnosis is based on histopathological and immunohistochemical findings; surgery remains the mainstay of treatment and careful follow-up is advised.
INTRODUCTION
Solitary fibrous tumor (SFT) is an uncommon neoplasm of mesenchymal origin, first described in 1931 [1]. Most SFTs are benign and their malignant potential is unknown. Surgery remains the treatment of choice and little is known about the benefits of adjuvant therapy [2–5].
We present a series of three cases – all women, ages 26, 40 and 78 years old – with a liver tumor discovered on abdomino-pelvic computed tomography, compatible with SFT, that were submitted to right, left and atypical hepatectomy, respectively. During follow-up, one of them presented metastatic disease, and another died with local recurrence.
As the rarity of this tumor makes its natural history unknown, careful long-term follow-up is advised [2].
CASE REPORT
Case 1
A 26-year-old woman, with past medical history of removal of hemangiopericytoma of the right leg, was referred to our Hepatobiliary Unit due to a liver tumor that was discovered on abdominal-pelvic computed tomography (CT) scan, performed after complaints of epigastric pain. CT scan (Fig. 1) showed a voluminous, heterogeneous, hypervascular mass, occupying segments 4, 5 and 8, with 19 cm in diameter, as well as suspicious lesion on left iliac bone suggestive of solitary fibrous tumor metastasis.
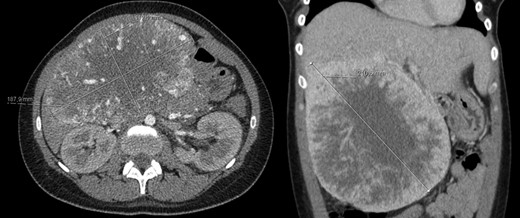
Abdomino-pelvic computed tomography (AP-CT) – voluminous heterogeneous liver mass in segments 4, 5 and 8 with 19 cm in diameter.
Right hepatectomy was performed on April 2011, followed by radiofrequency of the iliac lesion. Histology was compatible with solitary fibrous tumor.
Since then, the patient has undergone multiple interventions for the excision of metastatic lesions including: right pararenal lesion excision in August 2013 and radiofrequency of bone lesions (left iliac in 2011, D8 in 2012, again left iliac and lumbosacral spine in 2014, femur and right iliac bone in May 2015). In July 2015, diffuse bone metastasis, numerous secondary hepatic and para-cardiac lesions were diagnosed, systemic treatment with sunitinib was initiated. In March 2017, CT showed visceral progression, the patient started second line treatment with trabectedin, with stability of the disease till nowadays.
Case 2
A 40-year-old woman with past medical history of c-section at the age of 26, was referred to our Hepatobiliary Unit in 2013, with diagnose of liver tumor with 16.6 cm (Fig. 2) suggestive of solitary fibrous tumor.
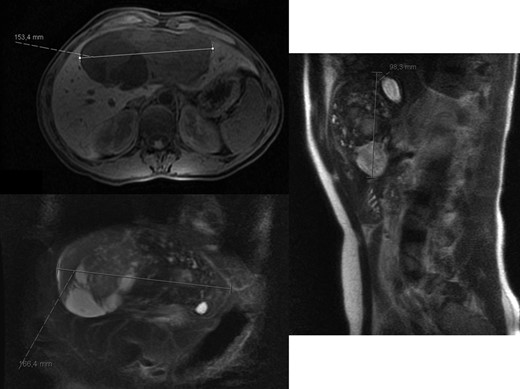
Abdominal Magnetic Resonance – heterogeneous liver mass in segment 4 with 16.6 cm.
No distant metastasis was identified.
A left hepatectomy was performed. Pathologic anatomy showed a well delimited nodular tumor, with 0.9 kg. On immunohistochemistry, the tumor cells were strongly positive for vimentin and CD34, confirming solitary fibrous tumor.
The postoperative course was complicated with biliary fistula requiring percutaneous drainage at 16th day postoperative and the patient was discharged home on 52nd day postoperative.
The case was discussed in a multidisciplinary meeting, clinical surveillance, with no adjuvant treatment, was decided.
At 56 months of follow up, the patient is asymptomatic with no evidence of recurrence.
Case 3
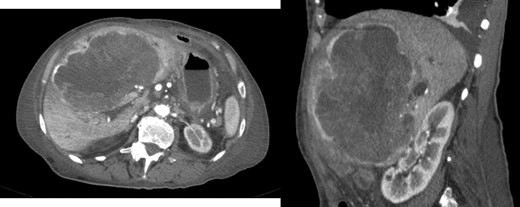
A 78-year-old woman with past medical history of hypertensive cardiopathy and bearer of a pacemaker, was referred to our Hepatobiliary Unit with diagnose of a liver mass discovered on CT scan, which was performed after complaints of nausea and postprandial infarction. CT scan (Fig. 3) showed a voluminous heterogeneous, lobed mass, displaying heterogeneous uptake contrast, relatively vascularized, localized in segment 1, with exophytic growth to the left lobe, with 18.5 × 13.8 × 15.6 cm; the tumor caused deviation of the stomach to the left.
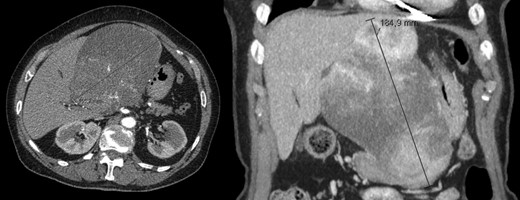
AP-CT – voluminous heterogeneous mass in segment 1 with 18.5 cm in diameter.
Atypical hepatectomy was performed. Pathologic anatomy showed, smooth outer surface and 2.2 kg weight. On immunohistochemistry, the tumor cells were strongly positive for vimentin, CD34, CD99, Bcl-2, and they were negative for SM-actin, supporting the diagnose of a solitary fibrous tumor.
At 16 months, follow-up, local recurrence was identified on CT scan, showing an expansive heterogeneous lesion, below the stomach, with 7.4 cm of maximum diameter, showing no cleavage plan with the stomach (Fig. 4).
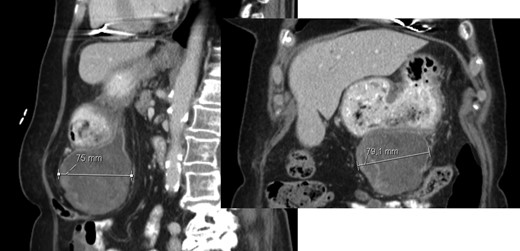
AP-CT – expansive heterogeneous lesion, with 7.4 cm, showing no cleavage plan with the stomach.
The patient was submitted to tumor resection with partial gastrectomy and segmental colectomy of the transverse colon.
The case was discussed in a multidisciplinary meeting; clinical surveillance, with no adjuvant treatment, was decided.
After 11 months of follow-up, the patient was admitted to the emergency room due to asthenia, nausea, vomiting and jaundice. CT scan reveal hepatic mass with 15.2 × 13.5 × 8.8 cm (Fig. 5) causing obstructive jaundice by compression of hepatic hilum.
Exploratory laparotomy was performed and non-resectability diagnosed intra-operatively. Biopsy confirmed recurrence of the disease.
Progressive deterioration of general state due to evolution of the disease and subsequent hepatic and renal impairment lead to respiratory failure and patient’s death.
DISCUSSION
Solitary fibrous tumor (SFT) is an uncommon neoplasm of mesenchymal origin, initially thought to involve exclusively the pleura, pericardium, and peritoneum.
Advances in pathology have led to better understanding of the histogenesis, tumor distribution, and the remarkable histologic heterogeneity of SFTs, now considered to be a pathologically diverse neoplasm of fibroblastic or myo-fibroblastic origin. Hemangiopericytoma and SFT form a histologic spectrum of fibroblastic type mesenchymal neoplasms with overlapping clinical, imaging and cytopathologic features. Although SFTs were thought to predominantly involve the pleura, it is now established that SFTs can originate in virtually any site of the body. The hepatic location is extremely rare and the incidence of these tumors is unknown [2–7].
The majority of diagnosed hepatic SFT were in adults (mean age: 57.5 years) and sex appears to be a risk factor, with greater incidence in females [2–4].
Hepatic SFT is usually asymptomatic until the lesion becomes extremely large, carrying out symptoms associated with local compression of neighbor structures, such as abdominal pain, early satiety, dyspepsia, distension or palpable mass. Other non-specific symptoms include fatigue, weight loss, nausea and vomiting. Nevertheless, some patients remain asymptomatic even with large lesions [3].
The definitive diagnosis is based on typical histopathological and immunohistochemical features. Histologically, SFT is composed of high cellular proliferation of spindle to ovoid cells, arranged in a storiform pattern, intertwined by collagen fibers of various thicknesses and with the immunohistochemical staining positive for CD34, vimentin, and Bcl-2 and negative for smooth muscle actin. These characteristics differentiate SFTs from other liver tumors, such as primary hepatocellular carcinomas (CD34 negative), leiomyomas (smooth-muscle actin-positive and CD34 negative) and mesotheliomas (vimentin positive, CD34 positive, cytokeratin positive). Although the CD34 antibody is not specific of SFT and can be positive in angiosarcomas and gastrointestinal stromal tumors, it remains highly characteristic of SFT [2, 4, 8, 9].
About 10–15% of SFTs behave aggressively, with metastatic spread and local recurrence [2–4].
Complete surgical resection is the treatment of choice. As the biological behavior of these tumors and the patients’ prognosis have not been well defined, careful follow-up is mandatory [2–4, 9].
CONFLICT OF INTEREST STATEMENT
None declared.



