-
PDF
- Split View
-
Views
-
Cite
Cite
Athanasios Christopoulos, Christina Ligoudistianou, Panagiotis Bethanis, Maria Gazouli, Successful use of adipose-derived mesenchymal stem cells to correct a male breast affected by Poland Syndrome: a case report, Journal of Surgical Case Reports, Volume 2018, Issue 7, July 2018, rjy151, https://doi.org/10.1093/jscr/rjy151
Close - Share Icon Share
Abstract
Poland syndrome is a rare congenital anomaly in which affected persons are born with missing or underdeveloped muscles on one side of the body. In this case study we present the case of a 28-year-old male with absence of all middle phalanges of the right hand and other rare anomalies, who underwent reconstruction with a new method that combines a mixture of adipose-derived mesenchymal stem cells and fat transfer. The patient’s restoration of the pectoralis area was aesthetically successful with no complications and remained unchanged even after 3.5 years. The proposed method represents an interesting reconstructive approach for treating Poland’s syndrome deformities.
INTRODUCTION
Poland syndrome is a rare congenital anomaly in which affected persons are born with missing or underdeveloped muscles on one side of the body, resulting in abnormalities that can influence the chest, shoulder, arm and hand. The extent and severity of these abnormalities vary among affected persons [1].
To date, any intervention that has been proposed, had serious disadvantages mainly in men. In women’s population the correction has fewer disadvantages, by using implants in the atrophic breast [2].
The use of silicone implants is currently a common practice to treat this problem in both genders [3]. Disadvantages of this technique is a possible asymmetry between the affected and the unaffected and that these implants cannot fully reconstruct the area close to the shoulder. Therefore, the aesthetic outcome of this type of reconstructive surgery may be mediocre or even poor.
Given the fact that many patients with Poland’s syndrome have reduced fat tissue in the chest area may deteriorate the aesthetic result, due to the limited soft-tissue coverage of the implant leading to an unrealistic result. However, the fat tissue deficiency could be used to the patient’s benefit in a surgical technique that is described above. Due to the poor aesthetic outcome of the previous technique most patients seem to prefer the preoperative situation.
A second technique involves customized implants for pectoralis major reconstruction; these implants are prefabricated with the use of moulage techniques that do not require a first stage surgical procedure, but the aesthetic result is rather poor [4].
A third technique involves the use of the latissimus dorsi muscle of the patient to reconstruct the pectoralis major [5]. The method is not preferred for male patients, because it is an extensive surgical procedure and post-operative scars can appear in areas that cannot be covered by clothing.
Another technique includes fat grafting, after autologous fat liposuction from various areas of the patient’s body [6]. This technique may be utilized in cases where excess of fat is available. However, fat tissue atrophy is a common manifestation of Poland’s syndrome.
Here we present a new technique, which is not expected to show all these disadvantages; we describe a case of Poland Syndrome in a 28-year-old male with absence of all middle phalanges of the right hand and other rare anomalies.
CASE REPORT
A 28-year-old male presented with several signs of Poland syndrome on his right. These defects of the pectoralis major, defects in the ribs and costal cartilages and webbing of the axillary fold, hypoplastic skin, and subcutaneous tissues. The patient’s rib cage also was unusually small. His height was 173 cm and weighting 64 kg (Fig. 1). And his chest was measured to be 90 cm. Routine laboratory assays were normal. Patient gave his written consent after being fully informed about its purposes. The recommended reconstruction is a novel method combing a mixture of adipose-derived mesenchymal stem cells and fat transfer.

Photo showing the 28-year-old male with absence of all middle phalanges of the right hand and other rare anomalies due to Poland Syndrome. Preoperative view appearance.
One microliter of abdominal adipose tissue was harvested from the patient, under local anaesthesia and AMSCs cells were isolated as previously described [7].
Stem cells were cryopreserved and stored in liquid nitrogen. About 2 weeks before the iterative application, cells were thawed, and culture expanded. Finally, 28 × 106 mesenchymal viable stem cells administered intravenously, and sample’s sterility was examined (BacT/Alert, Biomerieux)
First session June 2014: Harvesting was performed by conventional lipoaspiration at –0.5 atm with 3 mm cannula from abdomen, waist and buttock areas. The purified fat (230 ml) was mixed with the stem cell culture and transferred at the pectoralis major muscle zone. Fat was injected into the soft tissues without invading intercostal spaces. Cephalosporin was administered intravenously as a prophylactic antibiotic 1 h before the surgery. Following the operation antibiotics were administered per os for 5 days.
Second session February 2015: Following the same steps 150 ml of purified fat were produced (derived from inner, outer and anterior thighs), mixed with a new stem cell culture and injected to the same recipient zone. The same instructions and antibiotic therapy were followed.
DISCUSSION
As mentioned above, several surgical procedures for aesthetic correction have been used for Poland syndrome with many side effects.
Recently, Yang et al. [8], proposed that the autologous fat tissues injection after squeezing centrifugation yields promising results since centrifugation would allow the selection of healthier cells, the patient’s own growth factors and extracellular matrix, and can also reduce complications from the destroyed old fat cells and the removed fluid triglycerides. The injected fat may also trigger stem cell differentiation specific at the affected area.
Several studies suggested that the presence of adipose-derived mesenchymal stem cells has clinical implications for autologous fat transfers because. These stem cells could contribute to the neovascularization by acting as endothelial progenitor cells and/or as angiogenic-factor-releasing cells [9, 10].
Thus, we injected a mixture of adipose-derived mesenchymal stem cells and fat transfer with (which resulted in) a post-operative period free of pain and highly satisfied aesthetic results. The patient was satisfied despite that the problem was still under correction. As presented in Fig. 2, 7 months after the second session a nearly complete symmetry was achieved. The outcome after 7 months after the second session remained inalterable after 3.5 years. No complications were noticed, and no benign growths were developed (lipomas, cysts, etc.). Furthermore, the soft tissue thoracic ultrasounds 3.5 years after the procedure (Fig. 3) showed that the lipid mass at the contraction area is like the regular one, and the patient’s satisfaction was very high. In conclusion, with the procedure that we used, we exploited to the maximum the limited adipose tissue that we had as autograft since it is known that Poland’s syndrome is characterized by fatty tissue atrophy, and our results suggests that the stem cells seems to contribute to the survival of a higher percentage of fat.
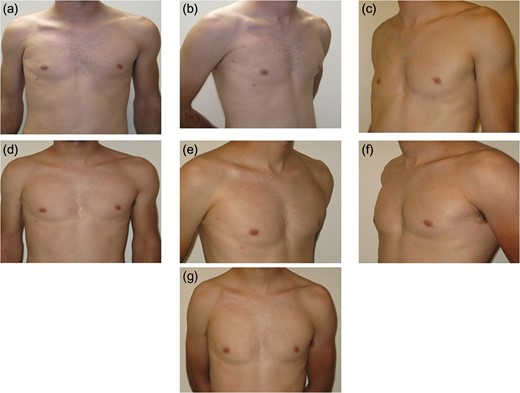
Serial photos showing the changes between 2 months after the first surgery and 3.5 year follow-up: (a–c) View 2 months after the first surgery. (d) View 4 months after the first surgery. (e) 8 months after the first surgery. (f) View 7 months after the second surgery. (g) View 3.5 years after the reconstructive procedure.
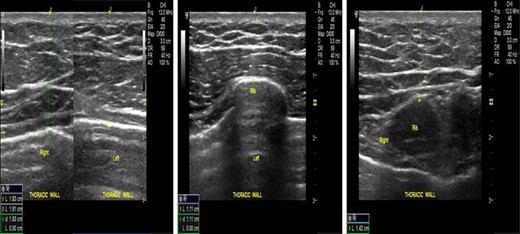
Serial soft tissue thoracic ultrasound photos 3.5 years after the first surgery indicating no pathologic findings.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



