-
PDF
- Split View
-
Views
-
Cite
Cite
Nolan R Bruce, Zachary W Tilley, Jacob T Carlson, Juan Camilo Barreto Andrade, Management of T-cell large granular lymphocyte leukemia and concurrent retroperitoneal liposarcoma, Journal of Surgical Case Reports, Volume 2018, Issue 7, July 2018, rjy142, https://doi.org/10.1093/jscr/rjy142
Close - Share Icon Share
Abstract
T-cell large granular leukemia (T-LGL) is a rare lymphoproliferative disorder characterized by the clonal expansion of cytotoxic T lymphocytes. We present a unique case of T-LGL and concurrent retroperitoneal sarcoma occurring in a patient with long-standing rheumatoid arthritis. Pathology revealed a high-grade dedifferentiated liposarcoma. The diagnosis of T-LGL with a synchronous retroperitoneal sarcoma is a case that highlights the surgical management of these two rare conditions.
INTRODUCTION
T-cell large granular lymphocytic leukemia (T-LGL) is a rare disease with an estimated incidence of one case per 10 million individuals [1]. Approximately 25% of cases are diagnosed in individuals with rheumatoid arthritis (RA). In a case series of patients with T-LGL, 29% of patients were reported to have an associated neoplasm, more commonly of hematologic etiology [2]. Presenting symptoms, such as recurrent infections, are primarily related to the profound neutropenia often seen in these patients. Findings of anemia, thrombocytopenia, and B symptoms (fever, night sweats, weight loss) have also been described. Felty’s syndrome is an autoimmune disease characterized by splenomegaly, neutropenia, and rheumatoid arthritis and likely represents a diagnosis along the same spectrum of disease as T-LGL, demonstrated by the finding that 85–90% of cases of Felty’s syndrome and RA-associated T-LGL are HLA-DR4 positive [3].
The diagnosis of T-LGL is made by peripheral blood analysis, which demonstrates an increased number of T-cell large granular lymphocytes. As this is often an indolent disease, treatment is reserved for symptomatic patients with moderate to severe neutropenia, recurrent or complicated infections, transfusion-dependent anemia, or those with a co-existing rheumatologic disease necessitating therapy. Treatment of T-LGL is primarily with immunosuppressive agents, such as methotrexate with or without prednisone [4]. Splenectomy is usually reserved for those with symptomatic splenomegaly, though splenectomy may be considered in patients with severe anemia or neutropenia as this has been shown to improve hematologic parameters [5].
Approximately 15% of sarcomas originate from the retroperitoneum. Retroperitoneal sarcomas (RPS) have an estimated incidence of 2.7 cases per 1 million individuals [6]. Liposarcoma is the most common histologic type to arise in the retroperitoneum. These tumors are often asymptomatic and incidentally identified on radiographic imaging. Symptoms are typically due to the mass effect of the lesion on adjacent organs and structures. Surgical excision remains the primary treatment for these lesions. Any soft tissue mass in the retroperitoneum should raise suspicion for a RPS, and resection should thus be considered. A modest survival benefit has been demonstrated in the debulking of primary retroperitoneal liposarcomas that are unresectable [7]. The role for adjuvant therapy has not been clearly defined for RPS. We present a novel case of T-LGL and concurrent retroperitoneal sarcoma in a patient with RA.
CASE REPORT
A 48-year-old male with RA presented with bilateral lower extremity rash and swelling, fevers, night sweats, anorexia and unintentional weight loss over the prior 2 months. Due to financial issues, the patient had stopped taking methotrexate for treatment of his RA two years prior to presentation. He was noted to have pitting edema with non-tender palpable purpura on both shins surrounded by non-blanching petechiae extending proximally to the knees. A firm immobile non-tender mass was palpable in the left lower quadrant.
Laboratory work-up revealed a white blood cell count (WBC) of 1.0 K/ul, an absolute neutrophil count of 680, and an absolute lymphocyte count of 310. He was anemic with a hemoglobin of 6.9 g/dl. Rheumatoid factor was elevated to 180 IU/ml. An antinuclear antibody screen was positive at 1:320. Computed tomography (CT) of the abdomen and pelvis showed an enlarged spleen and a large heterogeneous mass in the left abdomen extending into the pelvis (Figs 1 and 2). A bone marrow biopsy showed abnormal CD3+ and CD8+ T-cell lymphocytosis with TCR(beta)+ and CD57+, consistent with the diagnosis of T-cell large granular lymphocytic leukemia.
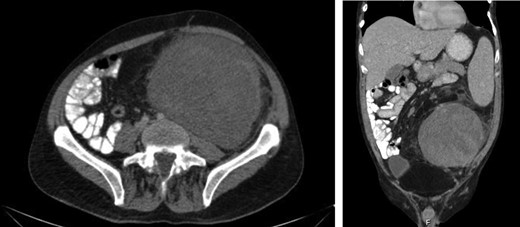
Axial and coronal CT images demonstrates the large retroperitoneal mass (50 × 33 × 16 cm) displacing bowel, the left kidney, left iliac vessels and bladder to the right.
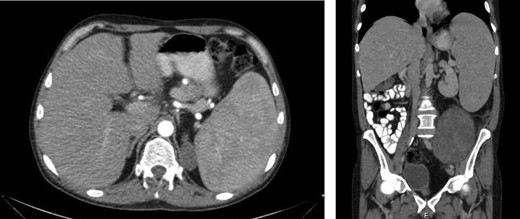
An enlarged spleen (16 × 10 × 22 cm) was identified on CT imaging obtained as part of the work-up of a palpable left abdominal mass.
The patient was evaluated by rheumatology, medical oncology and surgical oncology. He received 300 μg of filgrastim and was transfused two units of packed red blood cells pre-operatively. The patient was taken to the operating room for exploratory laparotomy and splenectomy. The left-sided retroperitoneal mass was vascularized by branches from the distal left external iliac artery and the left inferior epigastric artery. The retroperitoneal tissue was removed en-bloc extending from the splenic bed to the distal left external iliac, Gerota’s fascia to posterior abdominal wall, and lateral abdominal wall to the colonic mesentery (Fig. 3).

Pathologic analysis of the retroperitoneal mass returned as a high-grade dedifferentiated liposarcoma.
Pathology of the retroperitoneal mass returned as a 50 × 33 × 16 cm high-grade dedifferentiated liposarcoma arising in a background of well-differentiated liposarcoma. Margins were positive for dedifferentiated liposarcoma. The spleen was markedly enlarged (16 × 10 × 22 cm) but had no significant histologic change. The patient’s post-operative course was unremarkable, and he was discharged on post-operative day five, at which time his WBC count had improved from 1.37 K/ul with 21% neutrophils and 62% lymphocytes pre-operatively to 3.22 K/ul with 56% neutrophils and 17% lymphocytes post-operatively. CT imaging obtained nine months after surgical resection of the retroperitoneal mass shows no evidence of recurrence. Routine lab work demonstrates improvement in his anemia (Hgb 12.8 g/dl) and absolute neutrophil count (>1,500) while on maintenance therapy with methotrexate.
DISCUSSION
The treatment of T-LGL primarily involves the administration of immunosuppressive agents. Splenectomy should be considered in patient with symptomatic splenomegaly or patients with severe anemia or neutropenia [5].
RPS are often diagnosed as incidental findings on radiographic imaging unless they grow large enough to cause compression of surrounding organs or structures. The finding of a retroperitoneal mass should prompt consideration for excision even without a histologic diagnosis. Macroscopic total resection has been shown to have the greatest impact on overall prognosis, but the large size and diffuse nature of these tumors often make this challenging to accomplish. Mendenhall et al. [8] report that macroscopic total resection for RPS is achieved in about 50–67% of cases. Residual microscopic disease has been shown to increase the risk of local recurrence but has not been proven to adversely impact overall survival. T-LGL with concurrent retroperitoneal liposarcoma is a rare combination of diagnoses. This case highlights the nuances in the management of these patients.
ACKNOWLEDGEMENTS
The authors of this paper would like to acknowledge the University of Arkansas for Medical Sciences, particularly the Departments of General Surgery and Surgical Oncology, for their support in the production of this case report.
CONFLICT OF INTEREST STATEMENT
None.
FUNDING
The authors of this paper are the funding source for the preparation of this document. No outside sources of funding were utilized.



