-
PDF
- Split View
-
Views
-
Cite
Cite
Sean W Kaloostian, Tara K Vartanian, Christ Ordookhanian, Talia Vartanian, Paul E Kaloostian, Concomittant fibrous dysplasia with aneurysmal bone cyst formation within the skull, humerus and rib, Journal of Surgical Case Reports, Volume 2018, Issue 7, July 2018, rjy180, https://doi.org/10.1093/jscr/rjy180
Close - Share Icon Share
Abstract
Polyostotic fibrous dysplasia (FD) is a rare pathology characterized by the abnormal and gradual replacement of normal bone (calcium hydroxylapatite of osteoid matrix) with fibrous connective tissue. Aneurysmal bone cyst (ABC) is a tumor-like benign lesion with blood-filled cavities that can affect virtually any bone in the body. We report on a 20-year-old male presenting with an extremely rare pathology of FD with ABC formation of the skull, fourth rib and humerus. Our case report represents a novel literary addition to rare FD with ABC pathologies. Optimal diagnosis of this rare pathology can be achieved by a full body evaluation for clinical and radiographic FD with or without ABC, and optimal treatment for this rare pathology is the maximum surgical excision of the tumor and/or soft tissue.
INTRODUCTION
Fibrous dysplasia (FD) is a developmental bone disorder in which fibroblast proliferation results in excessive fibrous tissue replacing normal calcium hydroxyapatite of the osteoid matrix [1]. FD is a rare disorder representing 2.5% of osseous tumors overall [2]. FD may present in three forms with polyostotic FD accounting for 30% of cases. FD is a genetic bone disease with mutations in the GNAS1 (chromosome 20q13.2–13) gene of the osteoblastic lineage cells [3]. Mutations in the GNAS1 impairs the function of Gsα-GTPase which inhibits its ability to turn-off the adenylyl cyclase, producer of cAMP. Constitutive activation leads to increased rate of bone resorption seen within lesions of FD [1]. Aneurysmal bone cysts (ABC) are rare non-neoplastic, expansile and lytic bone lesions composed of multiple thin-walled communicating cystic cavities containing varying density blood [4]. Blood-filled cavities are lined by connective tissue with fibroblasts, osteoclasts and reactive woven bone, which is in turn rimmed with osteoblasts. Recent cytogenetic data reveals that ABC is a neoplastic pathology resulting from rearrangement of chromosome bands 16q22 and 17p13 which results in the formation of CHD11-USP6 fusion transcripts [5]. It is normal to find CDH11 in strong calcified bone, however, through oncogenic mechanisms, ABC patients express deregulate USP6 genes [5].
CASE REPORT
A 20-year-old male presented with painless right fronto-temporal forehead mass that was rapidly enlarging over a 4-week period. One month prior to presentation, our patient experienced intermittent headaches localized to the right fronto-temporal area unrelieved with analgesics. Our patient also noticed a rapid mass growth in the fronto-temporal area which upon was observed to be 5 cm × 5 cm, non-tender, and soft. Physical, neurological and laboratory assessments were all within normal limits.
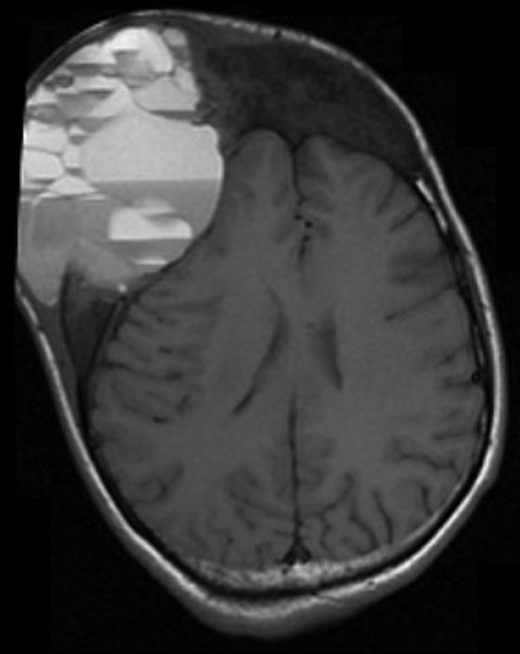
A computed tomography (CT) scan of the head 1-month after initial presentation revealed an aggressively appearing 5 cm × 5 cm soft tissue mass that was lytic and expansile involving the right frontal bone (Fig. 1). The lesion also involved the occipital bone with extension into the central skull base, nasal cavity and right nasal bone. Given the evidence of bone expansion and ground-glass appearance involving the calvarium, diagnosis was determined to be FD. Two weeks later, MRI studies revealed an aggressively enhancing 11 cm × 8 cm soft tissue mass with loculated fluid levels in the right frontal bone (Fig. 2). Extensive destruction of the outer table of the skull was noted with severe thinning of the skull inner table. Findings were thought to be consistent with ABC formation. Extensive bony involvement was noted primarily in the anterior and central skull base, but also in the occipital calvarium. Extension to the right zygoma and orbital walls with narrowing of the bony orbit was also visualized.

Four days later, the patient was admitted to the hospital for immediate drainage of the enlarging cystic mass on the right forehead and considered for either biopsy or excision of the skull lesion the following day. Cytology following cystic drainage revealed signs of acute inflammation without malignant cells. Upon admission, a CT maxillofacial scan with contrast revealed multiple areas of ground-glass appearance with extension of the skull base and decreased right optic canal.
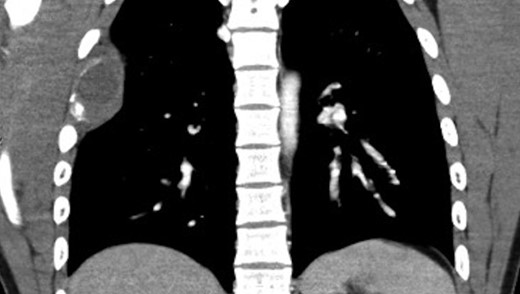
Chest x-ray revealed a destructive lesion in the posterolateral right fourth rib with associated soft tissue component consistent with FD. A CT of the chest revealed cortical thickening and ground-glass appearance of the right fourth rib (Fig. 3). A lytic lesion was noticed in the posterolateral fourth rib with a soft tissue component and cortical thinning adjacent to the area of FD appeared consistent with ABC. MRI of the chest revealed a 7 cm × 3 cm complicated cystic lesion within the right fourth rib with fluid levels consistent with ABC (Fig. 4). The skull lesion represented the most accessible site for biopsy and possible excision. For completeness, a bone scan was performed to evaluate other areas of involvement and remarkably the scan revealed increased uptake in the right frontal region, right fourth rib and in the right upper extremity. X-rays of the right upper extremity revealed non-expansile ground-glass process within the humerus and proximal one-third of the radius consistent with a history of FD with ABC formation (Fig. 5). The patient denied right extremity pain and was not tender to palpation along upper extremity.


The patient underwent a right frontal craniotomy for resection of dysplastic bone, removal of cyst and soft tissue tumor, and epidural decompression as a part of a joint effort between neurosurgery and plastic surgery. After peeling away the scalp, a large cystic component was visualized and removed within the lytic portion of the right frontal bone. Soft tissue components involved with the capsular mass were resected including areas of pericranium and temporalis muscle. A soft tissue component was also visualized to be lining the dysplastic lytic portion of the right frontal bone and was resected. The lytic bone along with soft tissue components lining the dura were then resected resulting in the final appearance of bare dura. Pathology of the right frontal capsular mass, pericranium, temporalis muscle and lytic bone were consistent for FD with secondary ABC. At the three-week follow up in clinic, the patient was well and had a noticeable head deformity. At the six-month follow-up, the patient demonstrated clear indications of proper recovery with plans for cranioplasty of the right frontal region.
DISCUSSION
Our patient presented with an extremely rare pathology of concomitant polyostotic FD with simultaneous ABC of the skull/skull base, humerus and rib. In literature, there exists many cases of polyostotic FD, but only a handful of FD cases with ABC (Table 1). In these few, no cases demonstrate concomitant occurrence of FD with ABC formation in three different locations throughout the body. Our report represents a novel case with multiple FD lesions with secondary ABC not seen in literature, highlighting the importance for a complete pre-operative work-up to determine the presence and extent of all lesions. Narrow-minded approach in cases similar to ours may result in overlooking pathology that is present and contributory to the greater well-being of the patient. Notably, surgical intervention and planning should be prioritized by symptomatic lesions first, followed by asymptomatic lesions.
Concomittant fibrous dysplasia (FD) with aneurysmal bone cyst (ABC) cases reports to-date
| Publication year . | Author . | Patient information . | Region involved . | Management method . | Follow up . |
|---|---|---|---|---|---|
| 1998 | Haddad et al. | Female, 6 years old | Skull base | Surgical resection | 4 Years, patient well |
| 2010 | Hadidy et al. | Male, 15 years old | Skull frontal bone | Surgical resection | None reported |
| 2011 | Terkawi et al. | Female, 7 years old | Sphenoid and ethmoid bones | Surgical resection | 5 Months, recurrent large tumor, parents denied treatment |
| 2011 | Sankaranarayanan et al. | Female, 6 years old | Maxillofacial | Surgical resection | 1 Year, patient well |
| 2016 | Urgun et al. | Female, 14 years old | Skull base to C2 vertebra | Surgical resection | ‘Regular follow up’, no duration listed |
| 2017 | Gotmare et al. | Male, 8 years old | Maxillofacial | Surgical resection | 6 Months, patient well |
| This case | Kaloostian et al. | Male, 20 years old | Skull and skull base, rib, and humorous | Surgical resection | 3 Weeks and 6 months, patient well, plans for future cranioplasty |
| Publication year . | Author . | Patient information . | Region involved . | Management method . | Follow up . |
|---|---|---|---|---|---|
| 1998 | Haddad et al. | Female, 6 years old | Skull base | Surgical resection | 4 Years, patient well |
| 2010 | Hadidy et al. | Male, 15 years old | Skull frontal bone | Surgical resection | None reported |
| 2011 | Terkawi et al. | Female, 7 years old | Sphenoid and ethmoid bones | Surgical resection | 5 Months, recurrent large tumor, parents denied treatment |
| 2011 | Sankaranarayanan et al. | Female, 6 years old | Maxillofacial | Surgical resection | 1 Year, patient well |
| 2016 | Urgun et al. | Female, 14 years old | Skull base to C2 vertebra | Surgical resection | ‘Regular follow up’, no duration listed |
| 2017 | Gotmare et al. | Male, 8 years old | Maxillofacial | Surgical resection | 6 Months, patient well |
| This case | Kaloostian et al. | Male, 20 years old | Skull and skull base, rib, and humorous | Surgical resection | 3 Weeks and 6 months, patient well, plans for future cranioplasty |
Concomittant fibrous dysplasia (FD) with aneurysmal bone cyst (ABC) cases reports to-date
| Publication year . | Author . | Patient information . | Region involved . | Management method . | Follow up . |
|---|---|---|---|---|---|
| 1998 | Haddad et al. | Female, 6 years old | Skull base | Surgical resection | 4 Years, patient well |
| 2010 | Hadidy et al. | Male, 15 years old | Skull frontal bone | Surgical resection | None reported |
| 2011 | Terkawi et al. | Female, 7 years old | Sphenoid and ethmoid bones | Surgical resection | 5 Months, recurrent large tumor, parents denied treatment |
| 2011 | Sankaranarayanan et al. | Female, 6 years old | Maxillofacial | Surgical resection | 1 Year, patient well |
| 2016 | Urgun et al. | Female, 14 years old | Skull base to C2 vertebra | Surgical resection | ‘Regular follow up’, no duration listed |
| 2017 | Gotmare et al. | Male, 8 years old | Maxillofacial | Surgical resection | 6 Months, patient well |
| This case | Kaloostian et al. | Male, 20 years old | Skull and skull base, rib, and humorous | Surgical resection | 3 Weeks and 6 months, patient well, plans for future cranioplasty |
| Publication year . | Author . | Patient information . | Region involved . | Management method . | Follow up . |
|---|---|---|---|---|---|
| 1998 | Haddad et al. | Female, 6 years old | Skull base | Surgical resection | 4 Years, patient well |
| 2010 | Hadidy et al. | Male, 15 years old | Skull frontal bone | Surgical resection | None reported |
| 2011 | Terkawi et al. | Female, 7 years old | Sphenoid and ethmoid bones | Surgical resection | 5 Months, recurrent large tumor, parents denied treatment |
| 2011 | Sankaranarayanan et al. | Female, 6 years old | Maxillofacial | Surgical resection | 1 Year, patient well |
| 2016 | Urgun et al. | Female, 14 years old | Skull base to C2 vertebra | Surgical resection | ‘Regular follow up’, no duration listed |
| 2017 | Gotmare et al. | Male, 8 years old | Maxillofacial | Surgical resection | 6 Months, patient well |
| This case | Kaloostian et al. | Male, 20 years old | Skull and skull base, rib, and humorous | Surgical resection | 3 Weeks and 6 months, patient well, plans for future cranioplasty |
ACKNOWLEDGEMENTS
Authors do not wish to disclose any acknowledgements.
CONFLICT OF INTEREST STATEMENT
All authors of this article declare no conflicts in any regard. All authors of this article did not receive any financial support or award for this completed study.



