-
PDF
- Split View
-
Views
-
Cite
Cite
Young Lee, Jasmine Bhinder, Sandeep Sirsi, Dhanan Etwaru, Armand Asarian, Philip Xiao, Unusual complication of bladder prolapse with subsequent diagnosis of urothelial carcinoma leading to a necrotizing soft tissue infection after radical cystectomy, Journal of Surgical Case Reports, Volume 2018, Issue 6, June 2018, rjy136, https://doi.org/10.1093/jscr/rjy136
Close - Share Icon Share
Abstract
There is lack of information in the literature on long-term complications of suprapubic catheters. The most common complications include urinary tract infection, bladder calculi, urine leakage and neoplastic changes. We report a case of an unusual complication of bladder prolapse, with subsequent diagnosis of urothelial carcinoma, leading to a necrotizing soft tissue infection after a radical cystectomy in a patient with long-term catheterization and its management. Due to the rarity of this complication, its management has not been well studied. In this particular case, the logical indication was radical cystectomy due to the presence of bladder necrosis.
INTRODUCTION
Suprapubic cystostomy (SPC) or suprapubic catheter is a thin tube surgically placed between the bladder and skin. Its primary purpose is to drain urine from the bladder in patients that have a lower urinary tract obstruction. Moreover, it is commonly used to manage neurogenic bladder secondary to spinal cord or other neurologic injuries [1–3].
Complications with SPC placement are well reported and include hematuria and bowel injury [1]. There is a lack of information in the literature on long-term complications of SPC. The most common complications include urinary tract infection, bladder calculi, urine leakage and neoplastic changes [1]. We report a case of an unusual complication of bladder prolapse with subsequent diagnosis of urothelial carcinoma leading to a necrotizing soft tissue infection after radical cystectomy in a patient with long-term catheterization and its management.
CASE REPORT
A 59-year-old paraplegic male presented to the emergency department with progressive prolapse of the bladder through his SPC site. He had a gunshot wound in 1990, which resulted in spinal cord injury and paralysis below T8, and in 2006, he underwent SPC to manage neurogenic bladder.
On presentation, physical examination revealed malodorous and necrotic appearing bladder mucosa protruding through the SPC site. Patient had associated diffuse abdominal pain but denied any fevers, flank pain, hematuria, increase or decrease in urinary output.
Patient consented to a cystectomy with an ileal conduit. A cystoscopy was performed prior to the procedure that revealed swelling and necrosis around the prolapsed bladder tissue. Multiple diverticula were noted, however, no stones or masses were appreciated.
The surgery was performed as a combined procedure by both the urology and the general surgery team without any complications. All of the necrotic tissue surrounding the prolapsed area were debrided until healthy tissue was encountered. The fascia was closed, however, the skin was left open due to the state of the prolapsed bladder through the skin. Packing was adequately placed with a wound vacuum assisted closure (VAC) over it. Patient was then transferred to the post anesthesia care unit in stable condition.
The histopathology of the bladder revealed stage IIIA (T3b) invasive and poorly differentiated urothelial cell carcinoma (Fig. 1) with areas of mullerian and squamous cell carcinoma features (Fig. 2). Histology also showed areas of necrosis and acute inflammatory changes.
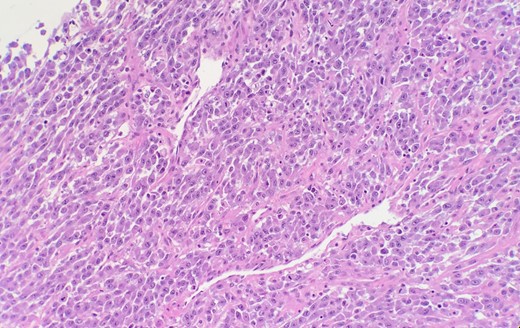
Microscopic examination reveals high grade urothelial carcinoma.
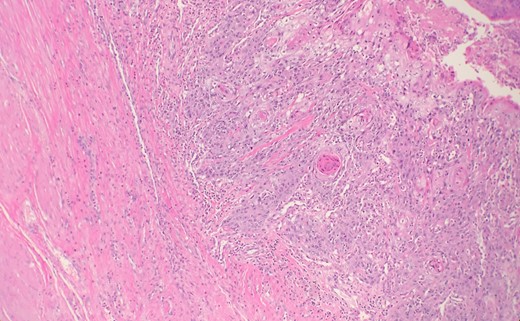
Microscopic examination reveals some areas show squamous differentiation with keratin pearls.
Six days after the operation, when changing the midline wound VAC dressing, bowel evisceration was noted at the lower aspects of the wound. Patient was taken back into the operating room that evening. The midline fascia was readily separated and remaining abdominal sutures were gently divided. Upon immediate inspection, the patient was noted to have necrotic fascial edges and subcutaneous tissue. Subsequently, using a combination of sharp dissection and electrocautery, the abdominal wall subcutaneous tissue was debrided. After successful debridement to attain healthy tissue margins, mesh was used to repair the fascial defect, as the fascia could not be re-approximated in a circumferential manner. After this was completed, the subcutaneous tissues were thoroughly irrigated and a new VAC dressing was placed. The abdominal tissue was sent to pathology and histology showed necrosis and microabscess formation.
Two days following the debridement and evisceration repair, the patient decompensated and a rapid response was alerted. At that time, the patient was febrile, tachycardic, hypotensive, short of breath and had altered mentation. He was intubated and started on fluids and antibiotics for treatment of acute respiratory failure secondary to septic shock.
Patient was brought back to the operating room for further debridement due to possible necrotizing skin infection. Necrotic mesh was removed and after adequate tissue debridement, an open abdomen negative pressure therapy system (ABTHERA) was placed over the abdomen.
Patient subsequently returned to the operating room on two additional occasions for further debridement secondary to continued necrosis of the abdominal wall. He remained intubated, sedated and on multiple pressors and broad-spectrum antibiotics.
Unfortunately the patient continued to decompensate and remained hypotensive with multi-system organ failure. Escalation of care was refused and only supportive care was continued.
DISCUSSION
Complications involving the placement of a SPC are well documented, however, there is limited data on the safety and long-term complications of an indwelling catheter [1–3]. A study by Nomura et al. reviewed 118 patients with neurogenic bladder after 5 and 10 years of SPC placement. In addition to the development of urinary tract infections, 25% of patients developed bladder calculi and 10% had leakage through the urethra, though no fatal complications were recorded.
A rare complication, which to our knowledge has only been cited in literature once, is bladder prolapse through the SPC site [4]. In the case reported, the patient was brought to the operating room and the prolapse was surgically repaired. In our patient, the prolapsed bladder was malodorous and necrotic. Subsequently, a decision to proceed with a radical cystectomy was made and histopathology of the bladder not only revealed necrotic tissue, but also, invasive urothelial carcinoma.
In conclusion, we present this rare case of necrotizing skin infection secondary to urothelial carcinoma from bladder prolapse through a patient’s SPC site. Due to the rarity of this complication, its management has not been well studied. In a previous case by Arkaprovo et al., a laparotomy was performed and the prolapsed bladder was repaired. Due to the presence of necrosis in our case, the logical indication was radical cystectomy.
CONFLICT OF INTEREST STATEMENT
None declared.



