-
PDF
- Split View
-
Views
-
Cite
Cite
Sebastião D de Morais, Bruno M Mikhael, Stephanie I A Németh, Isabella M L Paulo, Érico O H de Barros, Olímpia A T Lima, Burkitt’s lymphoma presenting as acute appendicitis: a case report, Journal of Surgical Case Reports, Volume 2018, Issue 6, June 2018, rjy131, https://doi.org/10.1093/jscr/rjy131
Close - Share Icon Share
Abstract
Appendiceal lymphomas are exceedingly rare, constituting around 0.015% of all gastrointestinal lymphoma cases. Burkitt’s lymphoma is the second most prevalent pathology, diagnosed in 25.9% of patients. We report a case of a 36-year-old male admitted with acute abdominal pain with 2 days of evolution, localized in the right lower quadrant associated with hyporexia, but no fever. On examination he presented abdominal tenderness on the right iliac fossa. A diagnosis of acute appendicitis was made clinically. At the post-operative follow up, 2 weeks later, he presented a low back pain of high intensity, associated with swelling of the abdomen, night sweats, daily fevers and weight loss. The histopathological exam of the appendix revealed diffuse and transmural lymphoid proliferation. Immunohistochemistry suggested high grade B-cell lymphoma indicative of Burkitt’s lymphoma. This patient was staged as a IVxB lymphoma and was submitted into polychemotherapy with a complete clinical response in 8 months.
INTRODUCTION
Primary appendix neoplasms are uncommon, found in ~0.5–1.0% of appendectomy specimens at pathologic evaluation. Within this group, the appendiceal lymphomas, which are exceedingly rare, constitute around 0.015% of all gastrointestinal lymphoma cases [1].
Burkitt’s lymphoma (BL) is a mature B-cell non-Hodgkin lymphoma with an aggressive clinical course [2]. A case series of 116 patients with appendiceal lymphomas determined that BL was the second most prevalent pathology, diagnosed in 25.9% of patients [1]. This rapidly growing tumor can cause symptoms due to mass effect or direct involvement of the bowel [3]. Patients affected by extra nodal intra-abdominal Burkitt’s tumor may have symptoms of bowel obstruction, intussusception or appendicitis [4].
Acute appendicitis is the most common presentation of primary appendix neoplasms [5]. Therefore, histological examination following appendectomy for an apparent appendicitis is essential and can provide the diagnosis of BL, which leads to the specific disease management.
CASE REPORT
A 36-year-old male was admitted with acute abdominal pain with 2 days of evolution, localized in the right lower quadrant associated with hyporexia, but no fever. On examination he presented abdominal tenderness on the right iliac fossa. The complete blood count appointed a discrete leukocytosis of 13 200/mm3 with no left shift. Lymphocyte count was within the standard. A diagnosis of acute appendicitis was made clinically. At operation, a Rockey-Davis incision was made in the right iliac fossa. The appendix was quickly identified, not adherent to any tissue. It had a thickened wall and a congested appearance, and there was no purulent liquid in the abdominal cavity. He was discharged 1 day after the surgical treatment fully recovered. At the post-operative follow up, 2 weeks later, he presented a low back pain of high intensity, associated with swelling of the abdomen, night sweats, daily fevers and weight loss. The histopathological exam of the appendix revealed diffuse and transmural lymphoid proliferation. Immunoperoxidase stains were positive for CD20, CD45, MPO, CD61 and KI-67 (expressed in 95% of lymphoma cells) and negative for CD3, BCL2, CD5 and MUM-1. Immunohistochemistry suggested high grade B-cell lymphoma indicative of BL, recommending further investigation with genetic testing for MYC gene translocation. Serology indicated positive IgG for both Epstein Barr virus/VCA and Cytomegalovirus, and negative for HIV. This patient was staged as a IVxB lymphoma and was submitted into polychemotherapy following the dose adjusted EPOCH-R (etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, rituximab) protocol with a complete clinical response in 8 months.
DISCUSSION
Primary gastrointestinal lymphomas are extremely rare, especially in the appendix. The most common extranodal lymphoma is diffuse large B cell lymphoma (DLBL), followed by BL. Studies suggest a higher predominance in males (81.9%) and white race (81%), compatible with this case [1]. BL involves a specific translocation involving the IgH and MYC genes in chromosome 14 and 8, respectively [2]. In this case report, the patient presented clinical findings compatible with acute appendicitis, which indicated urgent surgical approach without arising suspicion of another diagnosis intraoperatively. He only had a diagnosis of BL after histological and immunohistochemistry exams. This highlights the importance of mandatory careful histopathological examination of all appendectomy specimens.
The surgery was indicated at the moment of clinical diagnosis, dismissing any imaging techniques. Even though CT-scanning is not mandatory, it grants over 90% sensitivity and specificity for acute appendicitis and helps with other differential diagnoses [6]. In this case, the CT-scan was only solicited after the lymphoma diagnosis, revealing a bulky and extensive mass in the right iliac fossa, poorly delimited, along with right pyeloureteral dilation. A probable diagnosis of appendiceal neoplasms can be made based on the increased diameter of the appendix shown on CT-scans (>3 cm), which is out of proportion for a non-tumoral appendicitis [5]. The specificity for lymphoma increases when abdominal lymphadenopathy or aneurysmal dilation of the appendiceal lumen are present [7]. These findings corroborate with a pre-operative suspicion of a primary appendiceal neoplasm.
There is not enough data to suggest whether an aggressive surgical approach confers a greater survival benefit in contrast with a more conservative approach. A case series of 116 patients with appendiceal lymphomas had 69 (59.5%) patients submitted into an appendectomy and/or partial colectomy and 17 (14.7%) patients submitted into a right hemicolectomy or greater resection. The study showed no mean survival difference between these patients [1].
Other studies have suggested that surgery offers substantial complications and that it should not be the initial approach. A systemic review by Cirocchi et al. reported no overall survival benefit in between patients who were managed medically and those who received surgery. Moreover, it was noted that nonsurgical patients had a better outcome and concluded that chemotherapy should be the first treatment choice for patients with primary GI lymphomas. In addition, a series with 16 129 patients presenting primary GI lymphomas reported by Shannon et al. revealed that surgery did not provide greater survival benefit [8, 9]. Therefore, surgery should be reserved for cases that have an emergent character, such as and acute abdomen, like in this case. This patient had an appendectomy followed by a polychemotherapic protocol known as dose adjusted EPOCH-R. He had a complete remission in 8 months of treatment, as can be seen in Figs 1–4.
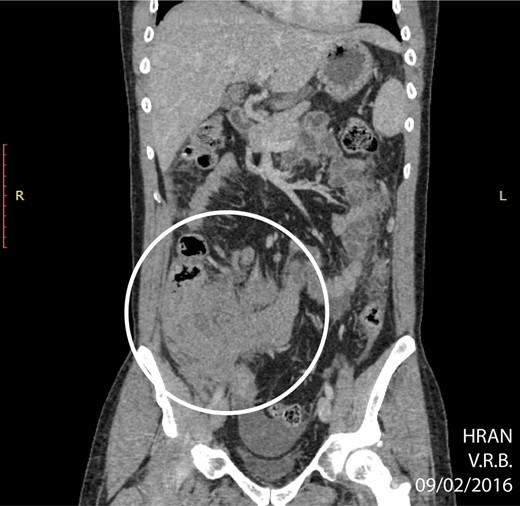
CT of abdomen (coronal plane) highlighting an extensive, ill-defined mass localized in the right iliac fossa (circle) (02/09/16).
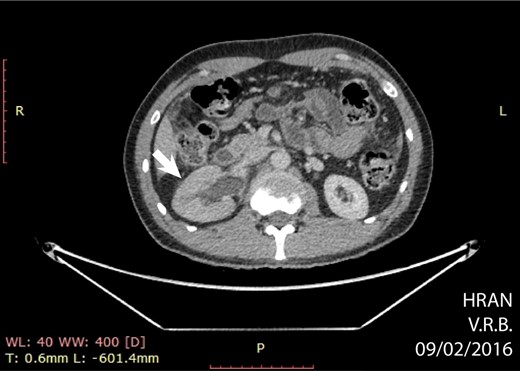
Axial CT showing hydronephrosis by compression of the tumor (arrow) (02/09/16).
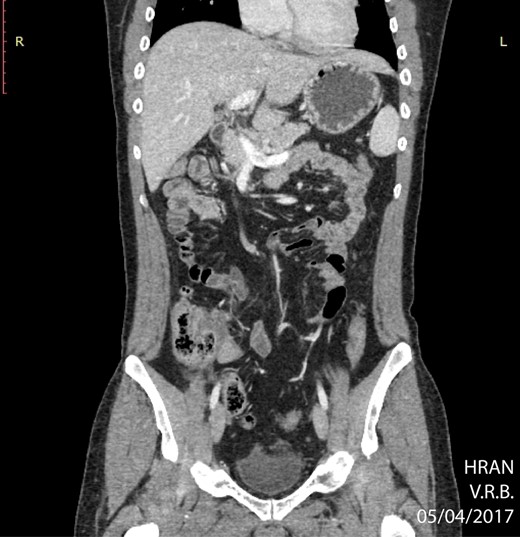
PET CT of abdomen showing regression of the abdominal mass (04/05/2017).

The surgical specimen. Macroscopy: thickened wall and congested appendix.
Appendiceal lymphomas are rare and difficult to diagnose. Acute appendicitis is a common presentation of such lymphomas and surgeons should always keep them in mind for differential diagnoses. Histopathological examination of all appendectomy specimens is highly encouraged. Surgery–chemotherapy combination is the best treatment option for appendiceal lymphomas when it presents as an acute abdomen.
CONFLICT OF INTEREST STATEMENT
None declared.



