-
PDF
- Split View
-
Views
-
Cite
Cite
Wahid Terro, Nizar Hamadeh, Miray Terro, Management of dermatofibrosarcoma protuberans of the face using lower trapezius musculocutaneous pedicle flap reconstruction: a case report, Journal of Surgical Case Reports, Volume 2018, Issue 6, June 2018, rjy089, https://doi.org/10.1093/jscr/rjy089
Close - Share Icon Share
Abstract
Dermatofibrosarcoma protuberans (DFSP) is a rare neoplasm which represents <0.1% of all tumors but it is considered the most common skin sarcoma. It is a slow-growing tumor that arises from the dermis and invades deeper tissues. The precise origin of DFSP is not well known. It is most frequently seen on the trunk, extremities, and head and neck. The standard treatment of the localized huge DFSP consists of a wide local surgical resection with recommended surgical margins of 2–3 cm. Local recurrence after incomplete excision is common. We present a case of 35-year-old man with enormous bulky mass on the face. Upon histological examination, the diagnosis of DFSP was made, and the patient underwent en bloc wide local excision of the mass followed by the use of Trapezius musculocutaneous pedicle flap reconstruction. On 32 months follow-up, no recurrence has been reported.
INTRODUCTION
Dermatofibrosarcoma protuberans (DFSP) is a very rare neoplasm of the dermis layer of the skin and is classified as a cutaneous soft tissue sarcoma [1]. The etiology of DFSP is not well known [2]. Scars caused by dermal burns, surgery or vaccination might increase the risk for developing DFSP [3]. DFSP tends to grow gradually and may initially present as a painless, skin-colored plaque with probable reddish brown or blue discoloration [2]. At later stages, it can increase in size and become protuberant [3, 4]. It usually appears in adults (25–50 years), but has been diagnosed in people of all ages and afflicts both sexes nearly equally [5].
DFSPs are mainly found on the trunk and the proximal extremities and at low percentage in the head and neck region [6].
Noteworthy, DFSP is often mistaken for other skin conditions such as lipomas, epidermal cysts and keloids in its early stages and for pyogenic granuloma and kaposi sarcoma in its later stages [7]. Tests and procedures used to diagnose DFSP comprise of clinical examination (incl. size and mobility), imaging tests (MRI to evaluate the tumor extent within the tissues and a CT scan to indicate bone invasion), and biopsy [8, 9]. Histological examination is the only definitive diagnostic method.
Treatment of choice for DFSP is wide local excision with negative margins of 3 cm from the tumor border (including the underlying skin, the subcutaneous tissue and fascia); and includes the periosteum or even a part of the bone in more complex cases [8]. One alternative to surgical resection is Mohs micrographic surgery with maximal conservation of tissue [8, 9]. Distant metastasis, however, is rarely reported [4].
CASE REPORT
A 35-year-old Syrian refugee presented with a large protuberant mass located on his face (Fig. 1). The patient reported an increase in the size of the tumor over the preceding 5 months and no changes following a drained incision of misdiagnosed facial abscess. He denied any recent, fever, night sweats and weight loss.
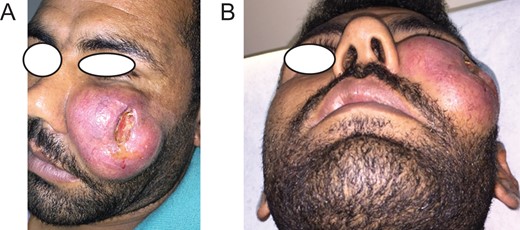
(A and B) A large protuberant mass located at the left side of the face of a 30-year-old Syrian refugee with skin laceration at the middle of the lesion.
Upon physical examination, a large, firm, painless, uni-nodular mass measuring (10 × 8 × 4 cm3) was found on the left facial skin with non healed incision in the middle of the mass ad with no sign of localized redness (Fig. 1). No palpable cervical or axillary lymph nodes were noticed.
Considering a possible diagnosis of a facial tumor, the patient underwent an incisional biopsy specimen. Based on the histological findings, the diagnosis of DFSP was made. MRI of the head and neck was performed showing a vascularized tumor. The patient was informed about the treatment plan which comprised of a surgical excision and reconstructive surgery. Upon approval of the treatment plan, a consent form was obtained. On 16 June 2015, under general anesthesia, en bloc excision of the mass with 3 cm margins was performed and a wound dress was applied. A final pathology review was employed to confirm negative margins (Figs 2 and 3). According to the report, no tumor cells were observed.
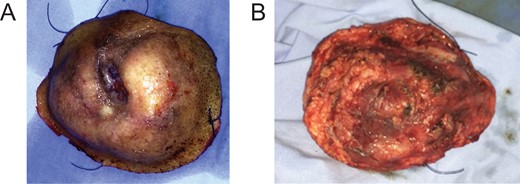
En bloc excision. Macroscopic appearance of the surgical specimen is that of a large tumor (10 × 8 × 4 cm3). (A) From outside view. (B) From inside view.
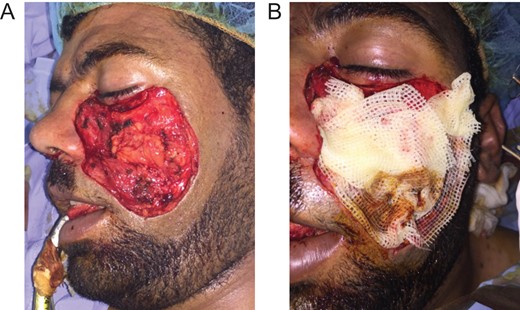
(A) Postoperative defect in the left cheek region. Bone exposure is well noticed. (B) The surgical field with a wound dress (16 June 2015).
Day 14 postoperative, given the size of the resulted defect and inability to adequately rotate local tissue, a lower trapezius musculocutaneous (LTMC) pedicle flap from the back was deployed (Figs 4 and 5). No further adjuvant therapy was required.
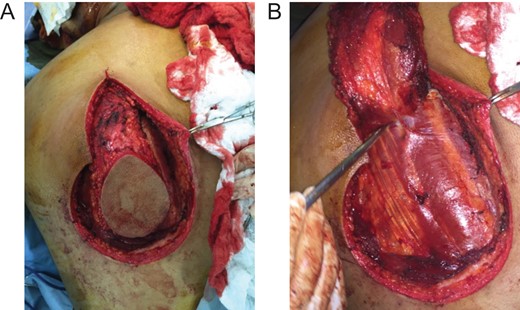
(A) Marking of the LTMC pedicle flap planning on the back. (B) Elevated flap as a distant pedicle flap. (30 June 2015).

The LTMC pedicle flap was completely covered the postsurgical defect (30 June 2015).
Day 42 postoperative, the flap was completely healed and succeeded in covering the defect (Fig. 6). The range of movement of the neck was limited with minimal medial–lateral rotation. A physical therapy and rehabilitation program was prescribed. After 2 months of intensive exercise, the performance of the neck improved.

Postoperative view of the well healed LTMC distant pedicle flap. Note the slightly depressed of the left lower eyelid (12 August 2015).
At 7 weeks, the donor site was completely healed (Fig. 7). At 32 months follow-up, clinical examination showed no signs of recurrence and the patient was actively using his neck.

Completely healed state of the donor site with secondary intention for 2 months.
DISCUSSION
DFSP is a rare malignant dermal tumor that originates from the dermis. The tumor accounts for <0.1% of all malignancies and for ~1% of all soft tissue sarcomas. The average tumor size has been reported to be ≤5 cm and tumors of 10 cm or more are extremely rare [2, 4].
The conventional treatment of huge DFSP (more than 5 cm) is radical wide local surgical excision—en bloc removal with abolition of 2–3 cm of uninvolved skin including the underlying subcutaneous tissue and fascia, and can extends to involve even muscle tissue if necessary to attain negative intact borders—with a recurrence rate of 8.8% (3). An alternative to extensive surgical resection is Mohs micrographic surgery with a recurrence rate of 1.5% (4, 8 and 9). Other types of treatment include radiation and targeted therapy [8–10]. In this report, the 10 × 8 × 4 cm3-sized tumor was entirely removed via en bloc wide local excision with margins of 3 cm. The excision included some branches of the facial nerve yet avoided the intraoral communication and the underlying bones, namely, the zygomatic bone. No further adjuvant therapy was necessary.
The use of local flaps to cover the resulted extensive postsurgical field was inappropriate. As such, the use of the extended LTMC pedicle flap for facial reconstruction was the best treatment of choice as it covered up all the area and facilitated wound healing. LTMC pedicle flap’s enormous arc of rotation allows its application for the immediate or late reconstruction of massive deformities following resection of tumors of the face. Moreover, it helps avoid major morbidity normally associated with such resections. In our case, histological assessment was the ultimate diagnostic means to confirm the diagnosis of DFSP. MRI was used to reveal the expansion. There was no evidence of recurrence after 32 months.
Wide local en bloc excision with at least 3 cm surgical margins in conjunction with the use of the LTMC pedicle flap is the most suitable surgical method for treating huge DFSP on the face and is highly recommended in similar cases. Long-term follow-up is crucial for detecting future recurrence.
CONFLICT OF INTEREST STATEMENT
None declared.



