-
PDF
- Split View
-
Views
-
Cite
Cite
Jordan W Greer, William C Beck, Avi Bhavaraju, Ben Davis, Mary K Kimbrough, Joseph Jensen, Anna Privratsky, Ronald Robertson, John R Taylor, Kevin W Sexton, Dilated cardiomyopathy secondary to acute pancreatitis caused by hypertriglyceridemia, Journal of Surgical Case Reports, Volume 2018, Issue 5, May 2018, rjy104, https://doi.org/10.1093/jscr/rjy104
Close - Share Icon Share
Abstract
A 30-year-old male presented to an outside facility with acute pancreatitis and triglycerides of 1594. He was transferred to our facility after becoming febrile, hypoxic and in acute renal failure with triglycerides of 4243. CT scan performed showed wall-off pancreatic necrosis. He underwent continuous renal replacement therapy and his acute renal failure resolved. He was treated with broad spectrum antibiotics and discharged. He developed a fever to 101 a week later and was found to have a large infected pancreatic pseudocyst. This was managed with an IR placed drain. This was continued for 6 weeks. He came to the emergency department several weeks later with shortness of breath and 3+ edema to bilateral lower extremities and lower abdomen. TTE performed showed an EF of 15%. He was diuresed 25 L during that stay. His heart failure was medically managed. We present this case of dilated cardiomyopathy secondary to acute pancreatitis.
INTRODUCTION
Acute pancreatitis (AP) as defined by the revised Atlanta classification, has three levels of severity based largely on organ dysfunction [1]. Mild AP has no organ dysfunction. Moderately severe AP has organ dysfunction that remains <48 h or local or systemic complications without organ failure >48 h. Finally, severe AP has persistent organ dysfunction >48 h.
According to Carr’s review, hypertriglyceridemia is an uncommon cause of AP in 9% of cases. However, AP is seen in 14% of patients with hypertriglyceridemia. Triglyceride levels of <1000 mg/dL should raise suspicion for other etiologies of AP [2]. Necrotizing pancreatitis occurs in 20% of patients with AP with a mortality rate of up to 30% [3].
Following a literature search of PubMed using keywords pancreatitis and cardiomyopathy, there were no published case reports of dilated biventricular cardiomyopathy associated with pancreatitis. It has been reported that pancreatitis can cause Takotsubo Cardiomyopathy (TCM) [4–10]. TCM is a transient disease with apical ballooning of the left ventricular wall during systole. The reported incidence is 2% of acute coronary syndrome diagnoses [6]. There are a few case reports of pancreatitis induced TCM. Those cases resolved with treatment of the pancreatitis [4, 5, 7].
CASE REPORT
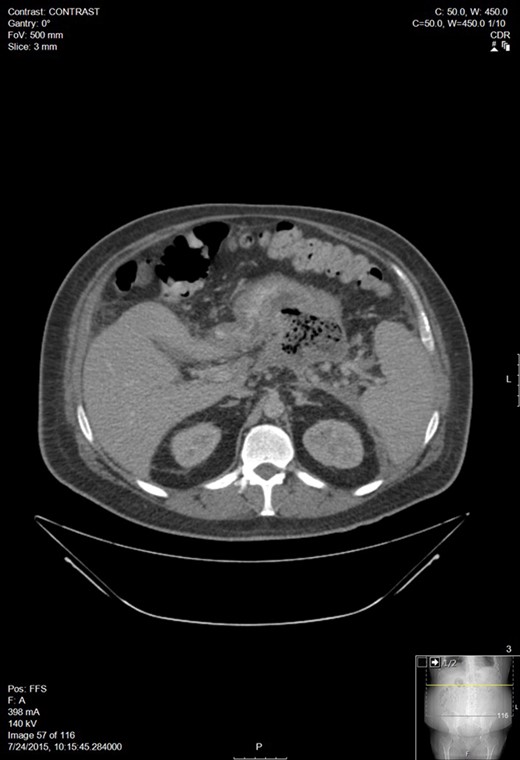
A 30-year-old man with a past medical history of hypertriglyceridemia presented to an outside ER with nausea, vomiting and abdominal pain. Lab studies were significant for pancreatitis (lipase 2730), hypertriglyceridemia (1594), blood glucose of 389 and BUN/Cr of 17/1.3. A CT of the abdomen showed AP. A subsequent lab draw showed BUN/Cr to 27/3.8, decrease in lipase to 565, increase in triglycerides to 4243, and a BNP 15. He was transferred to our facility following worsening hypoxemia. A CT scan was performed: representative sections shown below demonstrated walled off pancreatic necrosis (Fig. 1). He was in acute renal failure on presentation and started on continuous renal replacement therapy. The renal failure resolved, he completed a 7-day course of imipenem/cilistatin and was eventually discharged 11 days after admission.
A week later, he presented to his PCP for follow up and was febrile with increasing abdominal pain. CT of the abdomen and pelvis showed an 11 × 15 cm2 pancreatic fluid collection. His hemoglobin was 6.9 and he was transfused 3 units of PRBC. After transfer to our facility, a repeat CT showed a small pericardial and left pleural effusions, large volume ascites, a pancreatic fluid collection within the lesser sac between the anterior pancreas and posterior gastric body measuring 14 × 16.1 × 16.2 cm3, and blood in both paracolic gutters and pararenal spaces (Fig. 2). He was referred to Interventional Radiology for drain placement. After drainage, he clinically improved and was discharged.

Worsening walled off pancreatic necrosis with extension to the paracolic gutters.
His drains were followed in clinic and continued to drain necrotic material 6 weeks following initial placement. He refused laparoscopic necrosectomy, preferring to continue with non-operative management via the IR drains. Follow up MRCP revealed multiple intrabdominal fluid collections with the previous left-sided collection decompressing into the abdominal wall prompting another drainage by IR.
At his next appointment, he was having lower extremity edema and acid reflux. He was treated with leg wraps and a PPI. Approximately 1 week later, the patient presented to the ED for shortness of breath and increased swelling. On exam, he was found to have 3+ pitting edema up to his mid-abdomen. A chest x-ray showed bilateral pleural effusions and cardiomegaly. A TTE was performed which showed an EF of <15% and a moderate pericardial effusion without tamponade. He had elevated troponins, BNP of 2730, and elevated liver enzymes. CTA ruled out pulmonary embolism and showed a reduction in the left-sided abdominal abscess with some residual pockets of air. The patient was sent to IR for a drain check and US-guided paracentesis. Approximately 2700 ml of ascitic fluid was removed and a persistent moderate-sized abscess pocket with a fistulous tract of bowel was noted. He was diuresed almost 25 l during the hospital stay and discharged with medical management of his heart failure. His drains were removed when drain check no longer demonstrated a cavity or fistula.
He was followed in Cardiology clinic 2 months later with stable NYHF class I–II symptoms. A cardiac MRI was performed and showed enlargement of the heart with diffuse generalized hypokinesia consistent with dilated cardiomyopathy. With an ejection fraction of 22%. No evidence of myocardial infiltration. The patient remains in stable condition today.
DISCUSSION
Our case is unique, in that, despite resolution of the AP and subsequent pancreatic necrosis, the patient’s heart failure persisted. ECGs throughout the acute period of illness were normal except for sinus tachycardia. Imaging revealed no evidence of myocarditis or inflammation. There were no fistulous tracts visualized with MRCP to the pericardium as has been reported in prior case reports [10]. Our patient’s echocardiogram is not consistent with the normal findings seen in TCM. The multiple stressors over an extended period of time might contribute to the non-transient nature of our patient’s heart failure and could represent a new subgroup of TCM patients.
There is not a role for routine screening given the rarity of pancreatitis induced heart failure. More studies will need to be conducted to develop screening guidelines for patients with pancreatitis as there might be a subgroup that needs to be routinely screened. Further characterization of our patient’s heart failure could aid in elucidating a cause, however, he refused further studies. With so little published on pancreatitis induced heart failure and ~90% of TCM cases being postmenopausal women, we would not advocate routine screening for heart failure with BNP or baseline echocardiogram [5, 8, 9].
CONCLUSION
To our knowledge, this represents the first case report of a patient with dilated biventricular cardiomyopathy induced by pancreatitis.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- pancreatitis, acute
- antibiotics
- cardiomyopathy, dilated
- triglycerides
- hypertriglyceridemia
- edema
- computed tomography
- dyspnea
- heart failure
- hypoxia
- renal failure, acute
- fever
- emergency service, hospital
- pancreatic pseudocyst
- renal replacement therapy
- abdomen
- leg
- echocardiography, transthoracic
- pancreatic necrosis



