-
PDF
- Split View
-
Views
-
Cite
Cite
Jaime M Cevallos, Miguel A Moyon, Nelson E Pozo, Gabriel A Molina, Abdominal hernia and the unexpected final diagnosis, Journal of Surgical Case Reports, Volume 2018, Issue 5, May 2018, rjy099, https://doi.org/10.1093/jscr/rjy099
Close - Share Icon Share
Abstract
Mucinous neoplasm of the appendix are rare entities, among these, mucinous cystadenomas contribute to 31–34%. Cystadenomas often produce extensive dilatation of the appendix with epithelial atypia. Spontaneous perforation often occurs in 20%, leading to mucin distribution throughout the peritoneal cavity. Half of the patients are completely asymptomatic and are detected as an incidental diagnosis, others symptoms include a palpable mass, hernias, weight loss, peritonism or even intestinal obstruction. We present a case of a 71-year-old female, she presented with a palpable mass in the upper abdomen. A ventral hernia was the most likely diagnosis and hernioplasty was planned. At surgery, a mucinous mass was discovered and mucous material was found free en the peritoneal cavity. Also, a perforated appendix and a mass in the cecum was found. Patient underwent full recovery. Pathology reported pseudomyxoma peritonei as the final diagnosis.
INTRODUCTION
Abdominal ventral hernias are usually a fairly easy diagnose with a relative straight-forward treatment. However, in rare cases, some patients will have an undiagnosed pathology that could be missed. Pseudomyxoma peritonei is a rare disease that characterizes by the production and accumulation of mucous material in the abdomen. This mucous material can accumulate through an abdominal defect and could simulate symptoms indistinguishable from a hernia. We present a case of a 79-year-old female patient, she presented to surgical consultation with a mass in the abdomen. Ventral hernia was the most likely diagnosis and surgery was planned. Mucous material in the abdomen and a mass in the cecum was discovered. Pseudomyxoma peritonei was the final diagnosis.
CASE REPORT
Patient is a 79-year-old female patient with past medical history of hypertension, diabetes, hemorrhoidectomy and left total left knee replacement surgery. She presented to surgical consultation after having experienced a year of a mass in the upper abdomen. After physical examination, ventral hernia was the most likely diagnose, and surgery was planned.
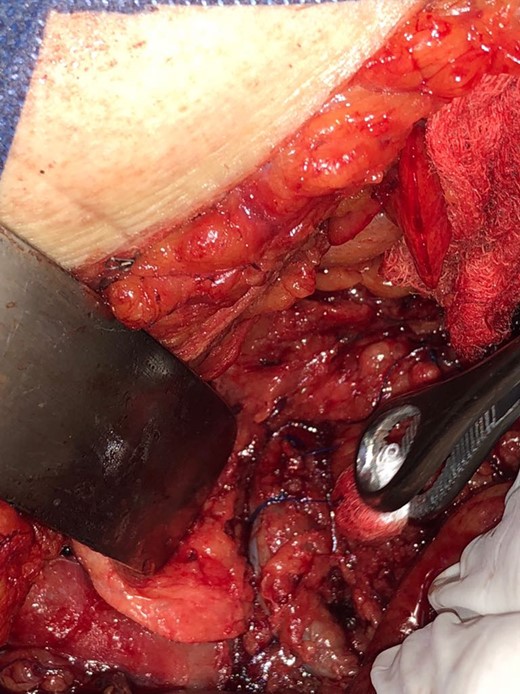
During the procedure, a 15 × 10 × 5 cm3 mucinous mass was discovered that was firmly attached to the subcutaneous tissue (Fig. 1A) that protruded from the peritoneal cavity through 6 × 6 cm2 aponeurotic defect (Fig. 1B). The mass was also attached to the greater omentum and mucous material was found free in the peritoneal cavity, most of it in the pelvic hole. Also, multiples adhesions were discovered that covered the transverse colon and the liver, ovaries appeared normal.

(A) Mucinous mass attached to the subcutaneous tissue. (B) Mucinous mass attached to the omentum that protrudes from the abdominal wall defect. (C) Right colon, with a perforated appendix and a mass in the cecum.
After exhaustive revision of the peritoneal cavity, a 3 × 3 × 1 cm3 mass in the cecum was also discovered, that compromised a thick appendix base and was covered with mucous material (Fig. 1C). The rest if the appendix was digested and mucous material was found instead.
The surgical decision was straight forward; the subcutaneous mass removed along with a part of the greater omentum. Also since the cecum was compromised, and the appendix was digested. A right hemicolectomy was performed and an ileocolic anastomosis was performed with autosutures. During the procedure, an adhesion between the transverse colon and the inferior vena cava was tractioned, and a severe bleeding occurred. However, due to prompt intervention, the lesion was identified and controlled (Fig. 2). A drain was left near the cava laceration, the aponeurotic defect was closed without a mesh, and the remainder of the surgery continued without complications
Pathology described a low grade disseminated mucinous cystadenoma of the appendix, the serosa of the cecum was congestive and infiltrated with mucous material (Fig. 3A), the base of the appendix was perforated (Fig. 3B) and was covered with mucous-hemorrhagic material (Fig. 3C). Pseudomyxoma peritonei was the final diagnosis.
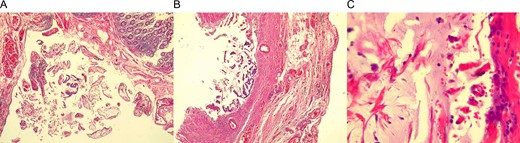
(A) Cecum wall, congestive and infiltrated with mucous material. (B) Appendix base, with atypia of goblet cells. (C) Mucous material covering the appendix base.
From there, the patient had good clinical development. Bowel sound and flatus were present from the third postoperative day. Which is why sips of liquids were initiated, attaining good oral tolerance, and low plus serous production of the abdominal drain. Soft diet was initiated and the drain was removed. The patient fully recovered from surgery. On follow up controls patient is well and was referred to the oncologist.
DISCUSSION
Mucinous neoplasm of the appendix are rare entities, contributing to only 0.2–0.7% of the appendiceal pathologies [1], and have a wide spectrum of clinical behavior, while invasive adenocarcinoma with malignant features is usually deadly, there are other mucinous neoplastic lesions that do not demonstrate invasive features, but still have the potential to spread, recur and metastasize, a clinical entity known as PMP [2].
Mucinous cystadenoma starts in the appendix with transformation of the appendiceal goblet cells and subsequent formation of a mucinous tumor [6]. This mucin accumulates and eventually perforate the appendix in ~20% [5]. When there is a perforation, mucin and cells escape in the peritoneal cavity, these cells lack surface adhesion molecules, exfoliate easily and passively circulate in the peritoneal cavity. They can deposit in the omentum, diaphragm and cul-de-sac [3]. This accumulating mucin increases the intra-abdominal pressure, and compress visceral organs [1, 3], it can herniate across an abdominal defect and simulate symptoms indistinguishable from a hernia in ~14% [8]. It can also promote inflammation with fibrotic response with the development of bowel obstruction [1, 3].
Clinical manifestations may be non-specific, and varied. From undistinguishable appendicitis to asymptomatic patients [8], it is also an unexpected finding in about 2 of every 10.000 laparotomies [4]. In our case, patient presented with an apparent abdominal hernia.
PMP appears in the seventh decade of life and is more common in females, 94% of cases of PMP develop from a mucinous tumor of the appendix [3], but it could appear from tumors from the stomach, gallbladder, colorectal and others [1, 3].
The best therapeutic approach should always be radical surgery, followed by cytoreductive surgery and hyperthermic intraperitoneal chemotherapy [5, 7]. Since most PMPs, appears from the appendix it should always be removed [3]. As it happened in our case.
If the PMP is discovered at the time of hernia surgery, the safest but most radical approach should be performed, appendix must be removed, samples must be taken, closure of the aponeurotic defect must be performed and the patient must be referred to an oncologic center.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- weight reduction
- epithelium
- appendiceal neoplasms
- cystadenoma
- cystadenoma, mucinous
- dilatation, pathologic
- hernias
- ventral hernia
- intestinal obstruction
- mucins
- mucus
- greater sac of peritoneum
- pseudomyxoma peritonei
- surgical procedures, operative
- abdomen
- cecum
- diagnosis
- pathology
- appendix rupture
- atypical
- spontaneous perforation



