-
PDF
- Split View
-
Views
-
Cite
Cite
Diganta Kakaty, Katharina Mueller, Falk Weippert, Roland Zengaffinen, Volvulus with bowel necrosis after laparoscopic appendectomy. Migration of Clip?, Journal of Surgical Case Reports, Volume 2018, Issue 5, May 2018, rjy093, https://doi.org/10.1093/jscr/rjy093
Close - Share Icon Share
Abstract
About 2.8% of patients develop small bowel obstruction, mostly following an open approach appendectomy. Case Report: we present an 18-year-old girl with acute abdomen 10 days following laparoscopic appendectomy. An emergency laparotomy was performed which revealed bowel necrosis and an impacted slipped clip on the mesenterial side of the bowel with signs of bowel strangulation and necrosis. Bowel resection was carried out with primary enteroenteric anastomosis. We suspect the sharp ends of the open clip allowed it to become lodged in the bowel segment resulting in bowel obstruction and subsequent necrosis. It is possible that the clip migrated or was a failed deployment. To our knowledge, this is the first report of mechanical bowel obstruction after laparoscopic appendectomy caused by aberrant surgical clip.
INTRODUCTION
Laparoscopic surgery is increasing in all specialties and ages. The rate of serious complications following laparoscopic appendectomy is overall low. The most common complications observed after surgical treatment of appendicitis are superficial and deep wound infections, prolonged ileus and pneumonia [1]. However, new and rare complications related to this procedure have been reported. Laparoscopic-related complications occur at the time of abdominal access for camera or port placement [2]. Complications can also arise from abdominal insufflation, tissue dissection and hemostasis [3]. The rate of postoperative small bowel obstruction following appendectomy (SBO) in adults is reported to be around 2.8%. The greatest risk factors for developing SBO are midline incision and nonappendicitis pathology [4]. We report a case of an adolescent girl presenting with bowel obstruction after laparoscopic appendectomy requiring exploratory laparotomy followed by a bowel obstruction 10 days later requiring ileocecal resection.
CASE REPORT
An 18-year-old female was admitted to our emergency room (Spital Visp, Spitalzentrum Oberwallis) on 16 May 2017 with abdominal pain, nausea and vomiting for 7 hours. The patient’s medical history reported heterozygote APC-resistance (factor V Leiden mutation), heterozygote mutation of factor II (positive family anamnesis) and asthma.
She had signs of peritoneal irritation on the right iliac fossa. The ultrasound examination showed a thickened appendix (7 mm), non-compressible, local ileocecal lymphadenopathy without perforation or abscess, consistent with acute appendicitis. The diagnosis was confirmed by laparoscopy and a laparoscopic appendectomy was carried out on the same day. Postoperatively, she was put on Rivaroxaban 10 mg for 2 weeks. There were no postoperative complications and after normal laboratory results, the patient was discharged after 2 days.
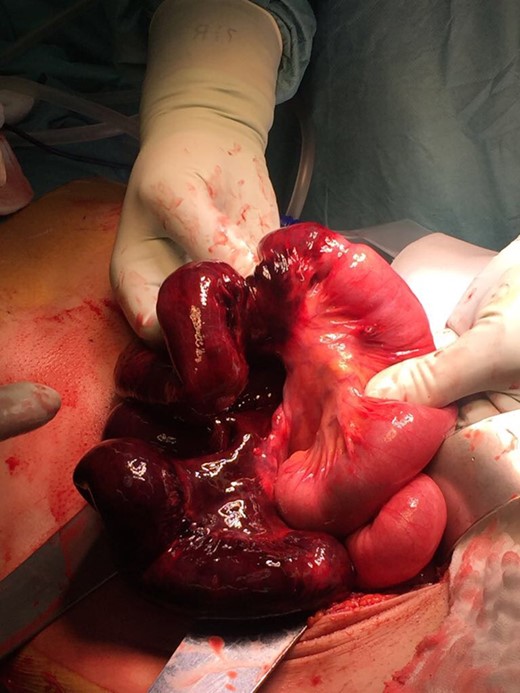
After 10 days, the patient was readmitted to our hospital with acute onset of periumbilical abdominal pain without associated nausea, vomiting, diarrhea, or dysuria. The clinical examination revealed silent bowel sounds and tenderness over the right lower quadrant without rebound tenderness. Vital signs were normal. Laboratory results showed elevated white blood cells with 12.0 G/l (4.0–10.0 G/l) and an elevated lactate with 4.8 mmol/l (0.50–2.20 mmol/l). Abdominal computed tomography was performed and showed loop distension and a large amount of free fluid. An emergency laparotomy was carried out. The surgical finding consisted of small bowel obstruction of the terminal ileum with necrosis along 60 cm of the small intestine. The necrotic bowel was then resected (ilea-cecal resection) and an enteroenteric anastomosis was performed. Interestingly we found a 6-mm metal clip, which was dislocated and wandered along the small intestine, most probably accounting for the source of volvulus. In the postoperative period, the patient evolved without intercurrences (Figs 1 and 2 ).
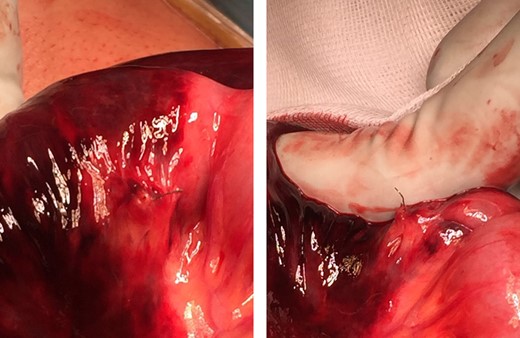
Impacted surgical clip on the mesenterial side of the small bowel wall.
DISCUSSION
Adhesions are the most common cause of bowel obstruction and are associated with prior laparotomy. About 2.8% of patients following appendectomy have been described as being associated with adhesive band formation and subsequent bowel obstruction [4]. Strangulation leading to ischemia, necrosis and ultimately perforation and sepsis are the most feared complication of small bowel obstruction. Although clinically, there is no way to determine strangulation, suggestive signs and symptoms of ischemia include continuous pain, fever, tachycardia, peritoneal irritation, leukocytosis and metabolic acidosis. It is generally accepted that immediate operation is required with a complete bowel obstruction. Intestinal obstruction with signs of strangulation or ischemia merits an urgent laparotomy. However, once conservative management is decided on, close observation of the patient is warranted. Worsening of patient condition or failure of nasogastric tube treatment could lead to a change in treatment plan and operative intervention as a definitive treatment.
Migration of a surgical clip causing intestinal obstruction after laparoscopic appendectomy is a very rare complication. Pub Med searches using the keywords ‘appendectomy,’ ‘surgical clip,’ or ‘bowel obstruction’ yielded no articles that matched this topic. On the other hand, many reports of complications from deviant surgical clips exist; most common is gallstone formation around a clip resulting in choledocholithiasis. Some of the more unique tales of aberrant clips include an open staple resulting in bowel perforation after laparoscopic-assisted vaginal hysterectomy; a surgical clip found in duodenal ulcer bed status after laparoscopic cholecystectomy; a surgical clip with erosion through the esophagus; stone formation around a clip resulting in nephrolithiasis; expectoration of a clip after pneumonectomy; and a surgical clip protruding through the urethra after radical prostatectomy [5]. This case report of volvulus with subsequent bowel necrosis resulting from a migrated surgical clip represents a unique tale in the ongoing history of aberrant surgical clips.
CONCLUSION
The patient in this case study presented with bowel obstruction after an abdominal laparoscopic procedure. Based on the history, it was suspected that the migrated surgical clip lodging in the abdominal wall was the likely cause of her small bowel obstruction. Ultimately, this guided the decision to choose a laparotomy as the definitive treatment in the patient with successful results (Figs 1 and 2).
CONFLICT OF INTEREST STATEMENT
None declared.



