-
PDF
- Split View
-
Views
-
Cite
Cite
Khuram Khan, Saqib Saeed, Amrita Persaud, Mohammad Sbeih, Sanjiv Gray, Leaque Ahmed, Retrograde jejunojejunal intussusception in a pregnant female after laparoscopic Roux-en-Y gastric bypass, Journal of Surgical Case Reports, Volume 2018, Issue 5, May 2018, rjy094, https://doi.org/10.1093/jscr/rjy094
Close - Share Icon Share
Abstract
Adult intussusception is a rare complication after laparoscopic Roux-En-Y gastric bypass (LRYGB) surgery. Incidence of intussusception is on the rise as the demand of bariatric surgeries is increased to treat morbid obesity. Among the bariatric surgeries, LRYGB gastric bypass results in significantly higher weight loss with thinning of the mesentery resulting in increased risk for intussusception. Majority of intussusception cases after gastric bypass have been reported in non-pregnant patients. We report a case of retrograde jejunojejunal intussusception in 6 weeks pregnant female following laparoscopic gastric bypass, which was diagnosed with abdominal magnetic resonance imaging and managed successfully with resection and revision of the anastomosis.
BACKGROUND
Laparoscopic Roux-En-Y gastric bypass (LRYGB) is one the most surgical procedures performed worldwide to treat morbid obesity and associated co-morbidities. Intussusception is a rare complication that is reported status post-LRYGB. The incidence of intussusception after LRYGB is 0.1 to 0.3% of the cases [1]. Intussusception is the prolapsing of a proximal segment of bowel (intussesceptum) into the lumen of the distal segment (intussuscipiens).
CASE PRESENTATION
A 37-year-old 6 weeks pregnant female status post-LRYGB 2 years ago presented with 4 hours history of sudden onset of epigastric and peri-umblical pain and tenderness, associated with nausea and vomiting. Vitals signs were stable. Labs including white blood cell count, serum chemistry, urinalysis and liver function tests were all within normal limits. Abdominal ultrasound confirmed intrauterine pregnancy. Magnetic resonance imaging revealed intussusception of small bowel with close loop obstruction (Figs. 1 and 2). Following initial resuscitation, emergent laparoscopy was performed which confirmed the diagnosis. Intra-operatively significantly dilated loop of jejunum approximately 20 cm in length was noticed close to the jejuno-jejunostomy with retrograde telescoping of the jejunum (Fig. 3). At that time decision was made to covert to open laparotomy with resection of irreducible intussusception and reconstruction of jejuno-jejunostomy (Fig. 4). Post-operative course was uneventful, the patient subsequently recovered fully and was discharged home on post-operative day 4. On follow-up, patient was seen in the clinic and reported doing well and pain free. Patient also was following up with her obstetrician to assess the viability of the fetus.
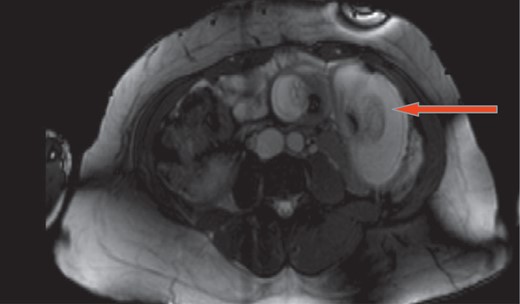
Magnetic resonance imaging shows intussusception of small bowel with close loop obstruction (cross section).
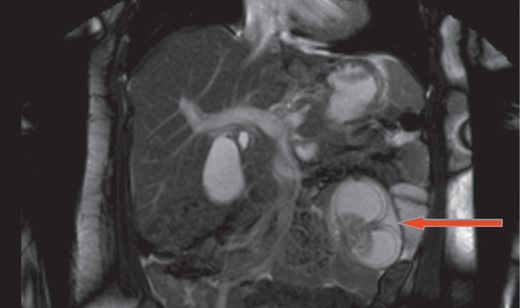
Magnetic resonance imaging shows intussusception of small bowel with close loop obstruction (coronal view).

Gross specimen showing resected; irreducible intussusceptions.
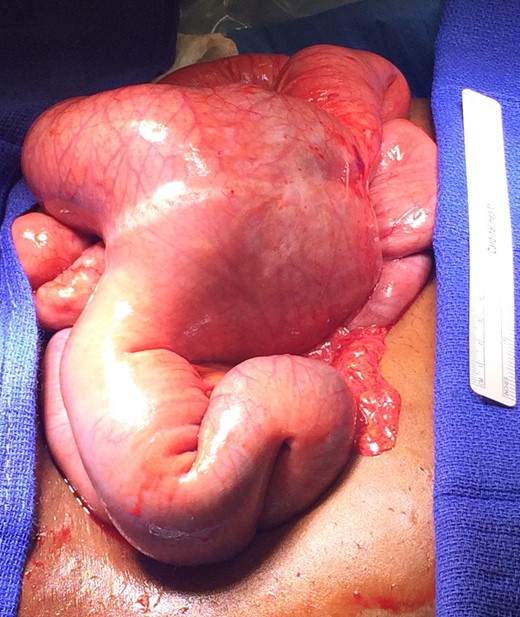
Gross image showing irreducible intussusception at the jejuno-jejunostomy.
DISCUSSION
Among the bariatric surgeries, LRYGB results in significantly higher weight loss. As weight loss occurs, fear of complications can arise. Post-LRYGB weight loss leads to thinning of the mesentery resulting in increased risk for intussusception [2]. The cause of telescoping of the intestine and prolapsing into one another and developing intussusception after gastric bypass is not clear. Some research suggests dysmotility as a cause of intussusception in post-gastric bypass patients [1]. As reported by Simper et al. after LRYGB that 0.1–0.3% of patients will get intussusception. Most intussusceptions are retrograde, but can be anterograde and located at the jejunojejunal anastomosis, which acts as the lead point [3]. Patients who are not pregnant, retrograde intussusception is more common [4].
After LRYGB intussusception is rare especially in pregnancy but if it does occur, it accounts for 5% of all intestinal obstructions [5]. Pregnant patients continue to lose weight after LRYGB surgery, it also improves their fertility. Index of suspicion for intussusception should be high in post-gastric bypass pregnant patients presenting with acute onset abdominal pain. In order to rule out intussusception a good history and physical exam along with ultrasound and magnetic resonance imaging (MRI) should be considered early in pregnant patients. The best imaging diagnostic test for intussusception is CT scan, however in pregnant patients it should only be done when the benefit outweighs the risks. Delay in the diagnosis can result in fatal outcome. MRI shows pseudokidney sign, with hypoechoic bowel wall mimicking the renal cortex and hyperechoic mesentery mimicking the renal fat in patients with intussusception. Once diagnosis of intussusception is made, next step is to perform diagnostic laparoscopy and reduce intussuscepted bowel. In other cases, if the intussusception is not reduced laparoscopy, conversion to laparotomy and resection and revision of the anastomosis should be performed.
CONFLICT OF INTEREST STATEMENT
None declared.



