-
PDF
- Split View
-
Views
-
Cite
Cite
Tatsuya Okamoto, Akane Sekiya, Tomoo Daifu, Ryuichiro Doi, Hisato Kobayashi, Primary jejunal Burkitt lymphoma in a child: ultrasonic detection, Journal of Surgical Case Reports, Volume 2018, Issue 5, May 2018, rjy090, https://doi.org/10.1093/jscr/rjy090
Close - Share Icon Share
Abstract
Gastrointestinal Burkitt lymphoma (BL) is a highly aggressive malignancy in childhood, and early treatment is critical for its favorable prognosis. Ultrasonography is a widely accepted initial imaging workup; therefore, recognition of the sonographic features of BL should contribute to its early diagnosis and initiation of treatment. We present a 4-year-old boy with primary jejunal BL with intussusception mimicking presentation, in which initial abdominal US allowed sustainable detection and characterization of the intestinal lesion. Jejunotomy was performed and histopathological analysis revealed a ‘starry sky’ pattern and c-myc split signals characteristic of BL. The patient remains disease-free following chemotherapy.
INTRODUCTION
Burkitt lymphoma (BL) is a highly aggressive cancer and the most frequent subtype of non-Hodgkin’s lymphoma in childhood. The gastrointestinal tract, especially the terminal ileum, cecum and appendix, are frequent locations of extranodal lesions of the sporadic BL found mostly in non-African patients [1]. The lesions also are reported occasionally as causes of pathological lead points (PLP) of intussusception [2]. Early imaging diagnosis of PLPs is, of course, crucial for the choice of reduction procedures, but also contributes to the prompt surgical diagnosis and early treatment of aggressive malignant diseases such as BL. Here, we report a case of primary jejunal BL with intussusception mimicking presentation, in which initial abdominal ultrasonography (US) allowed sustainable detection and characterization of the intestinal lesion.
CASE REPORT
A previously healthy 4-year-old boy presented with a 10-day history of intermittent abdominal pain, and 1-day history of nausea and vomiting. On examination, the patient had no fever and the abdomen was soft with slight distension. Supine abdominal radiograph demonstrated gaseous distension of small bowel loops in left-upper abdomen (Fig. 1a). Focused sonography was performed using a Toshiba Aplio 400 PVT-375BT transducer with the pediatric abdominal setting at a 5-MHz frequency. This revealed a circumscribed area of homogenously low echogenicity without wall stratification in the submucosal area of the intestine (Fig. 1b). Power Doppler sonography detected abundant blood flow signals in the same area (Fig. 1c). These findings prompted a strong suspicion of intestinal malignant lymphoma. The size of the lesion was ~20 × 5 mm2. A ‘target pattern’ was observed in the adjacent intestinal loops, and therefore intestinal intussusception with PLP was suspected (Fig. 1d). Subsequently, computed tomographic (CT) scanning of chest, abdomen and pelvis confirmed an intestinal intussusception in the left-upper quadrant (Fig. 1e), but no intraluminal mass was evident on US. There was no evidence of lymphadenopathy. Laboratory values showed an elevated level of soluble IL-2 receptor (sIL2R) of 854 U/ml. A decision to perform emergent laparotomy was reached owing to suspicion of irreducible jejunojejunal intussusception with malignant lymphoma and without extensive lesions. At laparotomy, although intussusception had already decreased spontaneously, there was a 2-cm intraluminal jejunal mass at a distance of ~70 cm from Treitz’s ligament. Mesenteric lymphadenopathy and other intestinal lesions were not evident and simple jejunotomy was performed. The post-operative course of the patient was uneventful.
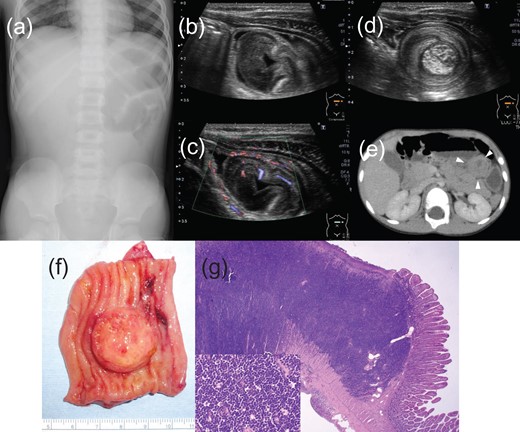
(a) Supine abdominal radiograph at initial presentation demonstrates a bowel gas pattern with gaseous distension of the left-upper small bowel loops. (b) Focused sonography of the abdomen demonstrates a well-circumscribed area of low echogenicity in the lumen of the intestine, (c) and power Doppler sonography detected abundant blood flow signals in that area. The lesion was ~20 × 5 mm2 in size. (d) A ‘target pattern’ was observed in the adjacent intestinal loops, which suggested intussusception. (e) CT scanning confirmed an intestinal intraluminal mass in the left-upper quadrant (white arrowhead). (f) Freshly exophytic tumor bulging into the jejunal lumen, involving half the circumference of the wall. (g) The tumor is composed of scattered pale tiny body macrophages on a dense background of monomorphic, intermediate-sized lymphocytes, creating a ‘starry sky’ pattern (lower left).
The resected specimen consisted of a 5-cm segment of jejunum. The intraluminal tumor was 20 × 20 × 5 mm3 in size (Fig. 1f). Histopathological examination with hematoxylin and eosin (HE) staining revealed a ‘starry sky’ pattern with abundant mitotic small cells (Fig. 1g). The cells stained positive for CD10, CD20, CD79a in immunohistochemical stains, confirming the presence of B-cells. Bcl-6 stain was also positive. TdT and BCL2 were negative. Ki-67 stain was positive in almost 100% of the tumor cells. Those findings were consistent with BL, as confirmed by paraffin-embedded tissue section fluorescence in situ hybridization (FISH) showing c-myc split signals. Post-operative positron emission tomography (PET) scanning identified intense foci of increased radiotracer uptake in the intestinal mesentery, which confirmed the diagnosis of stage III BL. The patient received chemotherapy according to JPLSG B-NHL03 protocol [3]. He remained free of evidence of recurrence during follow-ups.
DISCUSSION
Abdominal manifestation with intussusception is one of the major presentations of BL in childhood [4]. However, in a recent study, only three cases of BL were identified in 543 pediatric intussusception cases [5], which suggests that BL is actually rare as a cause of pediatric acute abdomen. US is a widely accepted initial imaging workup; therefore, recognition of the sonographic features of BL should contribute to its early diagnosis and treatment induction. In this case, that it is a (i) circumscribed [6, 7], (ii) submucosal uniformly hypoechoic mass [8, 9], (iii) without wall stratification [9] and (iv) abundant blood flow [10] signs matches the crucial sonographic characteristics for intestinal BL, which corresponds histologically to diffuse infiltration of lymphoma cells in intestinal submucosal layers. Those sonographic signs are rather clearly discernable in small-sized tumors, which is not the case with CT scanning detection as shown in this case. In the case of a relatively large-sized tumor, previously reported US signs such as a ‘doughnut sign’, or a ‘pseudo-kidney sign’ [1] might also provide a clue to the diagnosis. In addition, as shown in this case, the imaging feature of sporadic gastrointestinal mass with the lack of nodal disease will different BL from other forms of lymphoma. The physician should consider the benefits of initial sonographic imaging not only for solid organs, but for the detection of intramural lesions.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.



