-
PDF
- Split View
-
Views
-
Cite
Cite
Athanasios Syllaios, Antonios Koutras, Prokopis A Zotos, Sofia Koura, Pavlos Machairoudias, Anastasia Papakonstantinou, Nikolaos Bourganos, Aristotelis Liakos, Colovaginal and colo-ovarian fistula at a patient with asymptomatic diverticular disease, Journal of Surgical Case Reports, Volume 2018, Issue 4, April 2018, rjy085, https://doi.org/10.1093/jscr/rjy085
Close - Share Icon Share
Abstract
Colovaginal and colo-ovarian fistulas are rare entities that could be attributed to diverticular disease after an episode of acute diverticulitis. Τhey could initially be manifested with symptoms that lead patients to the gynecologist. Gynecologists should consider them in the differential diagnosis, especially after recurrent episodes of sinusitis. We report the case of a 51-year-old woman with a colovaginal and a colo-ovarian fistula due to subclinical diverticular disease, which should be involved in the differential diagnosis in those complicated fistulas, even if the patient had never before a clinical episode of acute diverticulitis or known diverticular disease, and a successful surgical approach.
INTRODUCTION
Colovaginal and colo-ovarian fistulas are rare entities. They are uncommon conditions with a few studies described in the current literature. Common causes of colonic fistula formation are: Crohn Disease, neoplasm, diverticulitis, previous surgeries, obstetrical injury, radiation injury, appendicitis and pelvic inflammatory disease [1, 2]. We report the case of a woman with a colovaginal fistula and an incidental colo-ovarian fistula due to subclinical diverticular disease. Our main objective is to present those rare entities and to raise physicians’ awareness, that, fistula formation due to diverticular disease could be achieved even in patients with asymptomatic diverticular disease and subclinical diverticulitis.
CASE REPORT
A 51-year-old woman was referred to the surgical outpatient department by the gynecologists because of stool and gas leaking through the vagina. The patient complained of recurrent urinary tract and sinusitis, as well as mucus vaginal discharge for ~2 months. She had received medication from her gynecologist for those symptoms, until stools started leaking. Her medical history was unremarkable; she had never undergone a colonoscopy, an abdominal surgery, hysterectomy, C-section, radiation treatment, traumatic injury, birth or hospitalization before. The physical examination was normal without signs of abdominal pain or palpable masses.
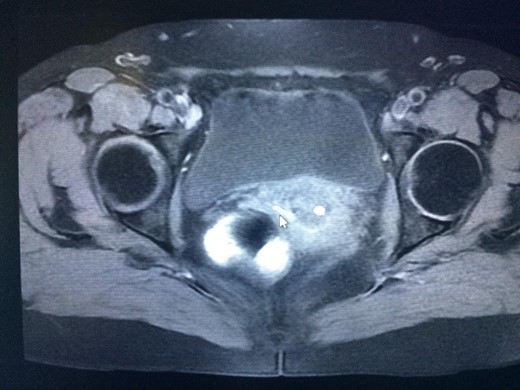
The colposcopy revealed a spot with inflammation at the left upper of the vagina, while the transvaginal ultrasound did not reveal any abnormalities. The colonoscopy did not reveal any tumor, but diverticulosis of the rectosigmoid colon with mild inflammation was found. The pelvic MRI showed multiple diverticula in the sigmoid colon, and one of them with a fistula tract of ~3 cm reaching the posterior wall of the vagina (Fig. 1).
At laparotomy, diverticulosis with a long fistula tract between one of the diverticula and the vagina (Fig. 2) and a short fistula tract between the sigmoid colon and the left ovary was found (Fig. 3). Low anterior resection, fistulectomy and left salpingo-oophorectomy were performed, while the vagina was sutured at the point of the fistula opening. The continuity of the bowel was restored with primary end-to-end anastomosis. The postoperative recovery was uneventful and the patient was discharged on postoperative Day 6. After 4 months of follow-up all the symptoms have resolved.
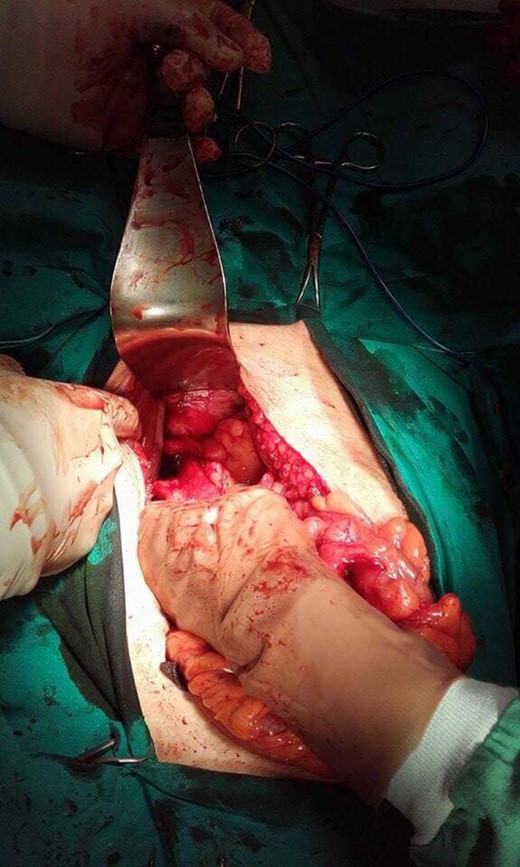
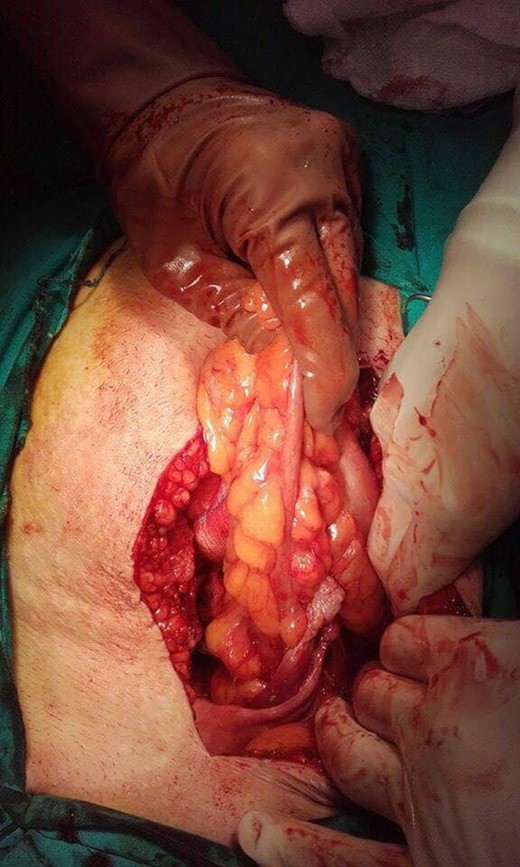
Pathological assessment of the specimen showed multiple sigmoid diverticulosis with two fistula tracts (3 and 0.8 cm) fistulized into the attached vaginal and ovarian tissues consecutively, with vascularized granulation tissue, acute and chronic inflammatory cells and foreign-body giant cell reaction.
DISCUSSION
Diverticular disease is a common manifestation between the elderly, especially for people older than 60 years. Among those with known diverticular disease, 10–25% will present at least one episode of diverticulitis. Complications of diverticulitis are: perforation (1–2% of patients with acute diverticulitis), phlegmon and abscess (30%), pylephlebitis (rarely), bowel obstruction (10–20%), bleeding (5% of people with colonic diverticulosis) and fistula (14% after an episode of acute diverticulitis) [3]. Most common colonic fistulas after diverticulitis are between the colon and the urinary bladder, the uterus, other intestinal segments, the skin, the vagina and the least often reported are with the fallopian tubes, the gallbladder and the ovary [2, 3]. The main hypothesis to the pathogenesis of a fistula is the breaching of the wall integrity of an adjacent anatomic structure from an abscess, and, the formation of adhesions during inflammation.
The clinical presentation of colovaginal fistula can be variable: passage of flatus or stool through the vagina, vaginal discharge, recurrent sinusitis and feculent odor [1]. Colo-ovarian fistula, on the other hand, initially can be manifested with lower abdominal pain, malaise, vaginal discharge, urinary tract infections, palpable masses and fever [2]. During colposcopy in colovaginal fistula, stool or granulation tissue can be found at the fistula site. Extravasation of contrast into the vagina during contrast enema can also confirm the diagnosis. Flexible sigmoidoscopy and colonoscopy can identify the fistula and rule out the possibility of a neoplasm. MRI has the highest sensitivity in detecting those fistulas [4]. Colo-ovarian fistula, on the other hand, are extremely rare and there is not a suggested preoperative imaging. Pelvic ultrasound, CT-scan, barium enema have been used in the diagnosis. Foci of gas within the ovary or air in the fallopian tube could be illustrated in a CT-scan [2].
The past decades colovaginal fistulas were treated with the three-stage operation approach. This approach involved proximal colostomy and drainage, then resection of the involved portion of the colon with end to end anastomosis, and finally stoma reversal. Nowadays, resection of the diseased colon and primary end to end anastomosis is preferred. In a series of 60 women with colovaginal fistulas due to diverticulitis, 57 patients underwent surgery. From these patients, 47 had colovaginal fistulas, two colo-uterine fistulas and eight multiple fistulas. Sigmoeidectomy with primary end to end anastomosis was performed in the vast majority of patients (n = 51). The other six patients were managed with Hartmann’s procedure [5]. Laparoscopic approach is feasible, although it involves a high risk of conversion [6]. On the other hand, colo-ovarian fistulas are an extremely rare complication of colon diverticulitis with only a few cases reported in the literature. Because of the rarity of this complication there is not an established approach [2]. Resection of the involved colon with oophorectomy should be performed. Primary colon anastomosis is the procedure of choice [7]. Hartmann’s procedure could be performed as an alternative approach for patients with bad general condition and risk factors for anastomotic leak. Laparoscopic en-bloc resection of the diseased colon and the ovarian fistula has been reported. This approach reduces the recovery period [2].
In conclusion, colovaginal and colo-ovarian fistulas could initially be manifested with symptoms that lead patients to the gynecologist. Gynecologists should consider them in the differential diagnosis, especially after recurrent episodes. Those complicated fistulas could be attributed to diverticular disease, that should be involved in the differential diagnosis, even if the patient had never before a clinical episode of acute diverticulitis or known diverticular disease. Fistulas presenting with symptoms are most often treated surgically.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



