-
PDF
- Split View
-
Views
-
Cite
Cite
Mirko Ragazzo, Diletta Trojan, Lisa Spagnol, Adolfo Paolin, Luca Guarda Nardini, Use of amniotic membrane in the treatment of patients with BRONJ: two case reports, Journal of Surgical Case Reports, Volume 2018, Issue 4, April 2018, rjy073, https://doi.org/10.1093/jscr/rjy073
Close - Share Icon Share
Abstract
The use of bisphosphonates has led to a new disease, bisphosphonate-related osteonecrosis of the jaw (BRONJ). There is currently no effective treatment for this disease; the surgical approach is controversial. The widespread use of human amniotic membrane (HAM) in surgery and the results obtained have highlighted its many potential properties, including antimicrobial, anti-inflammatory, antifibrotic and antiapoptotic, as well as its capacity for encouraging epithelialisation and cell differentiation. These properties are believed to encourage the recovery of patients with BRONJ, facilitating the wound healing process after surgical debridement of the bone. We report our experience with the use of HAM: two patients treated with patches of HAM. The follow-up to date, which includes x-rays and clinical assessments, demonstrates good levels of epithelialisation and absence of infections and pain. To conclude, the use of HAM in patients with BRONJ seems to be a promising therapeutic alternative to current conventional treatments.
INTRODUCTION
Bisphosphonates (BPs) were first synthesized in the 1800s, but it is only in the past 40 years that they have been used to treat patients with bone disorders, particularly patients affected by oncological and haematological diseases [1–3] and benign metabolic bone diseases such as osteoporosis [4–6].
BPs have been employed in clinical practice for many years with good results, but one of the most serious complications of BP therapy is bisphosphonate-related osteonecrosis of the jaw (BRONJ).
Human amniotic membrane (HAM) is the inner layer of the fetal membranes and is widely used in surgical and medical applications as a versatile and useful biological dressing for wounds of various origins [7, 8]. The widespread use of HAM is attributable to its many potential properties: anti-inflammatory and antimicrobial, antifibrotic, antiapoptotic, immunomodulatory, epithelialization and cell differentiation–modulating capacities, inhibition of cancer cell proliferation and low immunogenicity [9, 10].
In this study we present two case reports where HAM was surgically used in patients with a diagnosis of BRONJ due to BP treatment, HAM patches were collected, processed and cryopreserved by Fondazione Banca dei Tessuti di Treviso onlus.
FIRST CASE PRESENTATION
An 85-year-old female patient was submitted by her regular dentist to the single extraction of tooth 46 in February 2016. The intraoral wound was subsequently slow to heal.
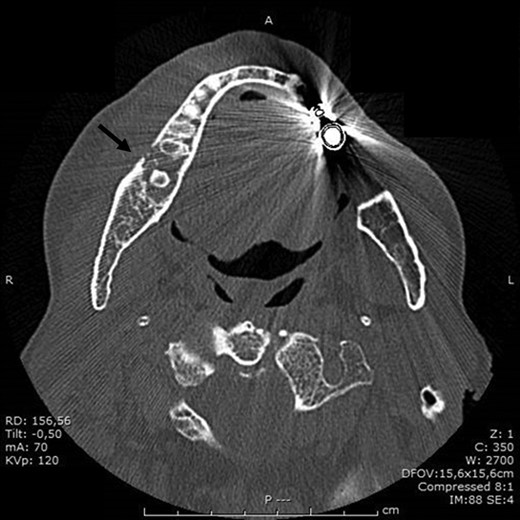
BRONJ was clinically diagnosed at the patient’s first visit based on her history and was confirmed radiologically by the dental x-ray and CT performed in July 2016. X-rays showed reduced density of the alveolar bone edges, particularly on the right where the alveolar bone crest profile was rather irregular. A small residual root was present in the molar region on the right. The inferior alveolar nerve canal was clearly recognizable, on both sides.
The residual root in position 46 was removed on an outpatient basis in August 2016 with sufficient antibiotic cover (amoxicillin + clavulanic acid). Dehiscence of the wound nevertheless occurred and the problem remained unresolved.
A bone biopsy pointed to acute exacerbation of chronic inflammation with lymphoplasmacytic and granulocytic infiltration.
In the light of these results, it was decided in September 2016 that the patient should undergo major surgery involving mandibular bone curettage and positioning of HAM (Fig. 1).

Prior to surgery, discontinuation of BPs was requested 2 months beforehand, with the possibility of resuming this treatment once the surgical sites had healed.
In November 2016, the patient underwent surgery under general anaesthesia. After infiltration of a local anaesthetic (mepivacaine + adrenaline 1:200 000), surgery was carried out as described: mucoperiosteal incision of the right mandible with mesial and distal drainage, extensive fistulectomy of the hyperplastic mucose membrane, which showed multiple fistulas, skeletonisation and exposure of abundant necrotic tissue; debridement of hyperplastic-inflammatory tissue and ostectomy of necrotic bone with osteoplasty of sharp edges; positioning of HAM and water and hermetic suture with Polisorb 3/0 absorbable braided thread (Fig. 2A–E). Histological examination confirmed the presence of inflammation and the diagnosis of osteonecrosis. The mesial and distal bone curettage margins were dictated by the x-ray images (Fig. 3) identifying above all the radio-opaque areas, often associated with a periosteal reaction, as well as by the need to remove any bone sequestra present. The imaging was also associated with the intraoperative assessment of the macroscopic appearance of the bone and in particular the signs of bleeding from the cortex and medulla. The HAM was 3 × 3 cm2 in size and was positioned over the curetted area and under the mucosal flap.
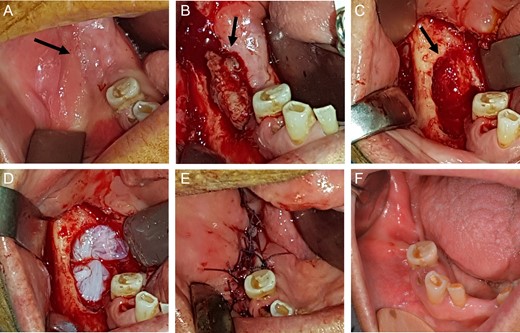
View of mandibular alveolar process in patient 1: (A) preoperative BRONJ affected area; (B) fistula, (C) curetted area, (D) HAM application, (E) suture of mucosal soft tissues and (F) postoperative follow-up after a period of 180 days.
The patient was submitted to a clinical and radiological follow-up 180 days after the procedure. The intraoral wound was completely sealed, the patient was asymptomatic and no further abscesses had developed (Fig. 2F).
SECOND CASE PRESENTATION
An 85-year-old male patient was submitted by his regular dentist to a single extraction of the painful tooth 35 in June 2016; the intraoral wound was subsequently slow to heal.
He was referred by the dental specialist to our outpatient clinic and was assessed by us first in September 2016 when objective examination of the oral cavity revealed a large area of exposed bone measuring ~2 × 1.5 cm2 in region 34–35.
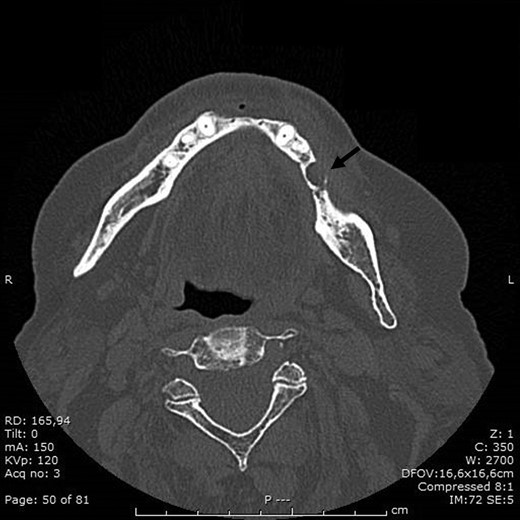
BRONJ had been clinically diagnosed at the patient’s first visit and confirmed radiologically by the dental x-ray and CT performed in September 2016, which showed marked demineralization of the anterior portion of the orbital ethmoid wall on the right, left mandibular osteonecrosis in the premolar region, a small periapical granuloma in position 44 and diffuse upper and lower alveolar atrophy.
A biopsy specimen was taken from the post-extraction alveolus in position 35 which revealed that the oral cavity mucosal fragment showed pseudoepitheliomatous hyperplasia associated with marked lympho-granulocytic inflammatory infiltration that was sometimes erosive, with aspects of inflammatory granulation tissue.
In view of the intraoral clinical picture and, in particular, of the incapacitating pain, it was decided that the patient should undergo surgery with mandibular bone curettage and positioning of HAM (Fig. 1).
Prior to surgery, discontinuation of BPs therapy was requested two months beforehand, with the possibility of resuming this treatment once the surgical sites had healed.
In November 2016 the patient underwent surgery under general anaesthesia (same technique used for the first patient described) (Fig. 4A–D). The mesial and distal bone curettage margins were dictated by the x-ray images (Fig. 5) which identified above all the radio-opaque areas, often associated with a periosteal reaction, as well as by the need to remove any bone sequestra present. The HAM was 3 × 3 cm2 in size and was positioned over the curetted area and under the mucosal flap.
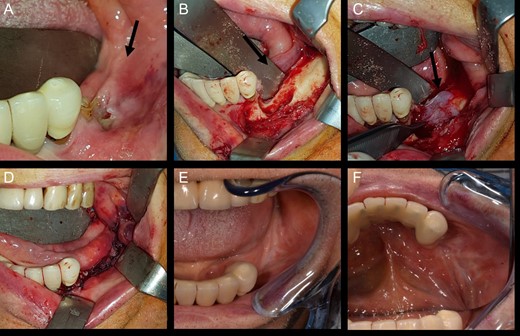
View of mandibular alveolar process in patient 2: (A) preoperative BRONJ affected area; (B) curetted area; (C) HAM application; (D) suture of mucosal soft tissues; (E) and (F) postoperative follow-up after a period of 180 days.
The patient was submitted to a clinical and radiological follow-up 180 days after the procedure (Fig. 4E and F). The intraoral wound was completely sealed, the patient was asymptomatic and no further abscesses had developed.
DISCUSSION
To date, the best treatment of BRONJ is still unclear; the idea of using HAM rather than other substances and/or healing aids was supported by the good results obtained.
The application of HAM can be viewed as a promising therapeutic alternative also for patients with BRONJ.
Based on the good results of these initial applications and the positive documented characteristics of HAM, it is possible to envisage using this tissue in the future also to treat other maxillofacial disorders involving overt healing problems as well as for pre-emptive purposes.
These encouraging results can provide a starting point for determining whether the application of HAM allografts can provide an promising therapeutic alternative, curative treatment in the future for patients with BRONJ, in terms of both pain reduction and definitive wound healing.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest regarding the publication of this article.
This study followed the Declaration of Helsinki on medical protocol and ethics.
FINANCIAL SUPPORT
None.



