-
PDF
- Split View
-
Views
-
Cite
Cite
Hyunyoung G Kim, Jennifer E Kesey, John A Griswold, Giant anorectal condyloma acuminatum of Buschke–Löwenstein presents difficult management decisions, Journal of Surgical Case Reports, Volume 2018, Issue 4, April 2018, rjy058, https://doi.org/10.1093/jscr/rjy058
Close - Share Icon Share
Abstract
Condyloma acuminata, or anogenital warts, caused by human papillomavirus are the most common sexually transmitted disease. In rare cases, the disease could progress to an extensive neoplasm called Buschke–Löwenstein tumor (BLT), also known as giant condyloma acuminatum. BLT differs from normal condyloma acuminata by presenting with locally invasive growth, lack of spontaneous resolution, tendency for recurrence after treatment and potential for malignant transformation. We examine a BLT case reaching large dimensions in the anorectal region treated with neoadjuvant chemoradiation therapy and surgical excision of residual lesions. Furthermore, continuous follow-up care can help identify and prevent recurrence or malignant transformation of the tumor.
INTRODUCTION
Since Buschke–Löwenstein tumor (BLT), or giant condyloma acuminatum, was first described in 1925, incidences of BLT have been reported in various anogenital regions [1, 2]. BLT is a slow-growing, cauliflower-like, locally destructive tumor that is caused by human papillomavirus (HPV) and has propensity for secondary infections, foul odor and fistulations [3]. With its relatively low-grade histopathological appearance and rare metastasis, BLT is generally classified as a verrucous carcinoma, a well-differentiated regional variant of squamous cell carcinoma [4]. A wide radical excision of the mass is considered the principal therapeutic intervention, and a regular follow-up is essential due to its frequent relapse and possible malignant transformation [5].
Our case presents a BLT with diffuse anorectal involvement that was treated mainly with chemoradiation therapy and to highlight the importance of follow-up care.
CASE REPORT
A 46-year-old male patient, of unknown sexual orientation, HIV-negative and history of alcohol abuse, was admitted to the hospital for diarrhea and purulent drainage of a foul-smelling, cauliflower-like lesion covering the bilateral buttocks. The patient had a history of multiple perianal condyloma acuminata that persistently recurred after a number of excisions and progressively enlarged over 20 years. On examination, a solid and fixed condylomatous lesion, measuring 27 × 20 cm2 (width × length) involved perineum, perianal area, and bilateral buttocks, from sacrum up to approximately the L4–L5 level. A fistula was also present along the right gluteal region, with the external opening measuring 2 cm in circumference and no signs of active infection. A computed tomography (CT) of the abdomen and pelvis showed a soft tissue density, measuring 14 × 11 × 17.7 cm3 (transverse × anteroposterior × craniocaudal), extending from the right posterolateral rectum, through the perirectal and presacral space, into the external buttocks (Fig. 1). Bilateral prominent inguinal lymph nodes were also noted. The colonoscopy showed involvement of the entire anal canal and rectum up to the distal sigmoid colon. The biopsy and histopathology showed condyloma acuminata with mild dysplasia and concluded a giant condyloma of Buschke and Löwenstein.
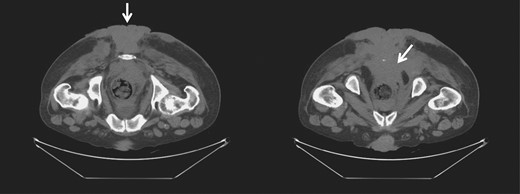
CT of the pelvis and perineum showing the BLT invading the rectum and anal canal.
While neoadjuvant chemoradiotherapy, with 5-fluorouracil, mitomycin-C and radiation dose of 45 Gy, at pelvic, perianal and gluteal regions was started, the patient was lost in follow-up. He was readmitted 2 months later for trouble controlling bowels, for which he underwent diverting colostomy. There was significant necrosis of the tumor (Fig. 2), and the biopsy showed with mild to moderate dysplasia. A wide local excision and debridement of the soft tissue were performed down to presacral fascia and gluteal fascia on right and left buttocks.
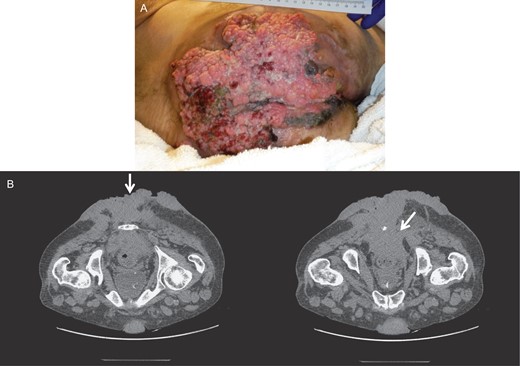
Gross image (A) and CT of the pelvis and perineum (B) showing exacerbation of the tumor with significant necrosis and invasion into the rectum and anal canal.
Four months later, after completion of the chemoradiotherapy, there was a significant resolution of the tumor (Fig. 3). No lesions could be felt on the rectal exam. The endoscopy and CT scan after another three months confirmed regression without presence of lesions. The scarred and necrotic soft tissue appeared to be residual from the chemoradiation and was debrided.
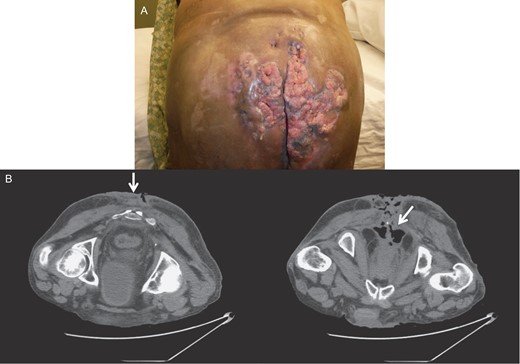
Gross image (A) and CT of the pelvis and perineum (B) showing tumor resolution and residual lesions after chemoradiation therapy.
However, ~6 weeks later, he was readmitted due to regrowth of the invasive anal condyloma. All of the areas previously quiescent and clean of tumor were full of new lesions, extending into the pelvic sidewall and the anorectal region, as well as the area of excision. The lesions deteriorated with necrosis, foul odor, and abscesses over time, and debridement and drainage were performed mostly to manage the wound and reduce septic risk (Fig. 4). Multiple readmissions for secondary infections and peri-lesion abscesses occurred for months.
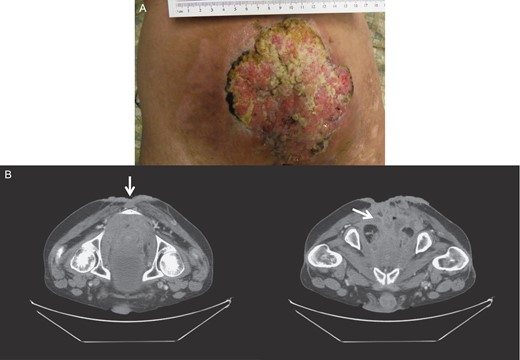
Gross image (A) and CT of the pelvis and perineum (B) showing tumor recurrence.
At the last evaluation, there were diffuse verrucal lesions in the anorectal canal. The patient also had extensive necrosis of in the presacral tissue between the rectum and anus, involving anal sphincter and perirectal fat, for which further debridement was performed. Biopsies confirmed severe dysplasia of condyloma. Ultimately, the tumor was determined to be non-curable and non-treatable, and the patient was placed on hospice care.
DISCUSSION
BLT is a rare sexually transmitted disease with an estimated incidence of ~0.1% in the general population with a 2.3:1 male to female ratio [6]. It is a slow growing, locally invasive and verrucous appearing tumor that does not spontaneously resolve. BLT resembles condyloma acuminatum histologically with its benign appearance and negligible cellular atypia, but also has characteristics of thick stratum corneum, marked papillary proliferation, deep local invasion and displacement of surrounding tissues [2, 7].
HPV, commonly low-risk strains 6 and 11 and occasionally high-risk strains 16 and 18, is known to be the etiologic agent [8]. However, the causal role of these strains in carcinogenesis has not been directly supported. The progression from condyloma acuminatum probably occurs during the immune suppression, such as congenital or acquired immunodeficiency, alcoholism, diabetes or chemotherapy with immunosuppressive therapy [9]. Our patient had a history of alcohol abuse, which likely contributed to consistent recurrence of genital warts and subsequent development of BLT.
Due to its rarity and lack of controlled studies, the optimal management for BLT has not been defined. However, wide local excision with tumor-free margins remains the treatment of choice along with several other therapeutic strategies, including topical agents (podophillin, 5-fluorouracil, bleomycin, interferon and imiquimod) or systemic therapy with chemoradiation [10]. Since the tumor has minimal potential for distant metastasis, local control of the disease usually leads to improved prognosis [9]. Moreover, APR is recommended in cases of multiple recurrences, malignant transformation, or invasion of the rectum, anal sphincters and pelvis5. This procedure, however, could not be performed in our case due to complexity of the closure of the perineal defect afterward.
Although surgical excision remains the mainstay treatment, definitive chemoradiation could possibly be used to treat certain cases of recurrence or extensive pelvic invasion, and potentially decrease local recurrence rates [10]. In our case, chemoradiatiotherapy proved effective and led to a significant resolution of the tumor. However, the recurrence could not be prevented, possibly due to inadequate assessment and surgical intervention, and the tumor deteriorated due to inconsistent follow-up care.
While vaccination is an effective method for preventing anogenital warts, early and adequate treatment of condyloma acuminata could prevent its potential growth into an extensive verrucous tumor. Early detection of the disease and close vigilance and follow-up could have led to a better outcome in our patient.
CONFLICT OF INTEREST STATEMENT
None declared.



