-
PDF
- Split View
-
Views
-
Cite
Cite
Wanding Yang, Michael Jones, Sameer Mallick, Tracheo-oesophageal fistula: a delayed complication of missed inhaled magnetic toys, Journal of Surgical Case Reports, Volume 2018, Issue 2, February 2018, rjy022, https://doi.org/10.1093/jscr/rjy022
Close - Share Icon Share
Abstract
Delayed diagnosis of tracheobronchial foreign body (FB) aspiration is not uncommon in children. It occurs when symptoms are underappreciated and/or radiological findings are overlooked. In such cases serious complications can arise, which make the diagnosis and removal of the FB much more difficult. Here, we present a case where FB aspiration was misdiagnosed as asthma after a radio-opaque FB on the chest radiograph was missed, leading to formation of a tracheo-oesophageal fistula as a rare delayed complication.
INTRODUCTION
Tracheobronchial foreign body (FB) aspiration is a leading domestic accident in children, under the age of 4 [1]. Delayed diagnosis or misdiagnosis can occur if children present with no history of aspiration or with atypical history of non-specific symptoms. This is associated with increased morbidity, such as recurrent pulmonary infection, atelectasis and bronchiectasis [2].
Here, we present a rare case of tracheo-oesophageal fistula as a delayed complication of aspiration of two small magnetic balls in a 3-year old girl. Her initial presentation was misdiagnosed as asthma after the radio-opaque FB in her first chest radiograph was mislabelled as a clothing artefact.
CASE REPORT
A 3-year-old girl was referred to the asthma clinic with a 3-month history of morning cough and wheeze. She was seen multiple times by her general practitioner (GP) who initially diagnosed her with upper respiratory tract infection. Her symptoms persisted despite salbutamol inhaler treatment so the GP organised a chest x-ray (CXR) (Fig. 1). It was reported that the left lung was translucent with reduced peripheral lung markings: finding consistent with asthma with bronchial plugging or a post infective bronchiolitis. It also showed a round radio-opaque FB over the left main bronchus. However, this was labelled as ‘Clothing Artefact’ on the actual radiograph and therefore did not alarm the GP or the reporting radiologist. A repeated PA CXR (Fig. 2) was undertaken in the asthma clinic where all clothes and hair were removed from the thorax. This confirmed the presence of a metallic FB in the left main bronchus and the patient was immediately admitted for bronchoscopy and removal of the FB.
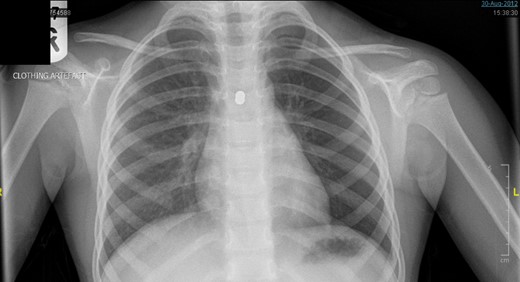
Initial posterior–anterior chest x-ray (CXR) demonstrated a translucent left lung with reduced peripheral lung markings. There is also a dense rounded foreign body projected over the left main bronchus. A label of ‘CLOTHING ARTEFACT’ was placed in the left upper corner of this CXR.
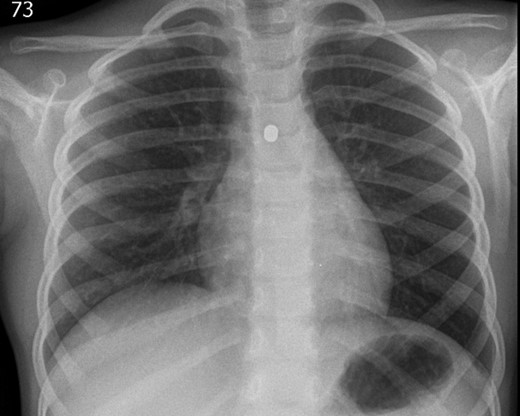
The repeated posterior–anterior CXR taken with all clothes and hair removed from the thorax of the patient. It confirmed the presence of a metallic foreign body in the left main bronchus.
A ventilating bronchoscopy was performed by the otolaryngology team where the FB was found to be stuck to the posterior wall of the left main bronchus. The FB was left in-situ. After the operation, a lateral CXR (Fig. 3) illustrated the metallic FB appeared to be two spherical balls, with the anterior one in the left main bronchus and the posterior one in the oesophagus. A subsequent further history from the parents suggested these were from the older sibling’s toys.
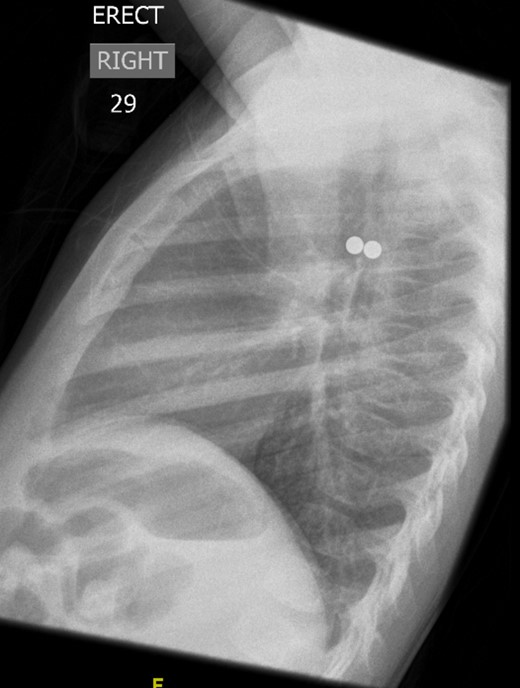
Lateral CXR showed the metallic foreign body to be two spherical balls, with the anterior one in the left main bronchus and the posterior one in the oesophagus.
Patient underwent another rigid bronchoscopy under the cardiothoracic team, which confirmed a tracheo-oesophageal fistula that had formed likely due to the slow migration of the metallic FB. The team proceeded to convert the operation to right thoracotomy where two pieces of stuck-together magnetic balls were found and removed. The tracheo-oesophageal fistula was repaired with a lateral costal flap. Water soluble contrast swallow post-operation showed no evidence of any residual fistula nor any contrast leak. The patient made a full recovery and was discharged 16 days after her initial admission.
DISCUSSION
Children of young age have a significant risk of FB aspiration as they tend to explore and place objects in their mouths. It frequently occurs before the fourth year of life, mostly likely as a result of inadequate dentition, the relatively high position of the epiglottis and the immature coordination of swallowing [1]. FB aspiration is considered a life-threatening emergency that requires prompt removal, but sometimes it may remain undetected because of atypical history or misleading clinical and radiological findings.
A convincing history and plain chest radiograph are the two main criteria for the diagnosis of FB aspiration [2]. Although FB aspiration may cause sudden airway obstruction and subsequent death, quite often symptoms are mild and non-specific. A history of initial choking and coughing episode with subsequent respiratory symptoms such as stridor and wheeze are immediately suggestive of the diagnosis. However, symptoms can subside spontaneously and quickly even when a FB remains [2]. Danger occurs especially when children fail to present with any history of aspiration. Instead, they may display symptoms and signs of unresolved or recurrent pneumonia as a consequence of chronic inflammation and tissue reactions caused by a long-standing FB [2]. Therefore, it is not uncommon for patients to be treated for other disorders, such as persistent fever, asthma or recurrent pneumonia for a long period of time before the diagnosis of FB aspiration is established. In our case, aspiration of the FB by the patient and the possible subsequent choking and/or coughing episode were not witnessed. She was conservatively treated with inhaler for a presumed upper respiratory tract infection for 3 months by her GP before the diagnosis became apparent on a repeated CXR.
Chest radiography as the first line investigation for suspected FB aspiration can prove the existence of radio-opaque FB and evokes the likelihood of FB aspiratory if it demonstrates hyperinflation, obstructive emphysema, atelectasis and/or consolidation [2]. However, these signs are inconsistent. In a series of 189 children with proven FB aspiration, 90 cases (48%) had normal chest radiographs [3]. What is striking in our case is that, in addition to the finding of hyperinflation of the left lung, the initial CXR demonstrated a round radio-opaque FB over the left main bronchus. Unfortunately, this was overlooked by both the GP and the reporting radiologist due to the incorrect labelling of ‘Clothing Artefact’ on the radiograph. As a result of delayed diagnosis, a tracheo-oesophageal fistula occurred for which the patient required open thoracotomy.
In conclusion, clinicians should always maintain a high index of suspicion for FB aspiration when patients of this age group present with acute or chronic respiratory symptoms and signs. Although labels such as ‘artefacts’ on radiographs are often useful to aid the interpretation of the image, suspicious artefacts should be explored and clarified early to prevent any obvious pathologies being missed during the diagnostic process.
Toys with magnetic parts have become popular among the paediatric population, and they are accessible to children because parents are not aware of their potential risks. The alarm has been raised previously about the risk of ingestion of magnetic toys causing intestinal obstruction and perforation [4]. We emphasize again the need for manufactures to highlight the hazards of magnetic toys on package to prevent the appearance of new cases.
CONFLICT OF INTEREST STATEMENT
None declared.



