-
PDF
- Split View
-
Views
-
Cite
Cite
Luke Nugent, Palanichamy Chandran, Need brooks no delay. Peritoneo-cutaneous fistula formation secondary to gallstone dropped at laparoscopic cholecystectomy 20 years previously: a case report, Journal of Surgical Case Reports, Volume 2018, Issue 2, February 2018, rjy013, https://doi.org/10.1093/jscr/rjy013
Close - Share Icon Share
Abstract
Dropped gallstones, in addition to inadvertent damage to the biliary tree, is a complication seen in laparoscopic cholecystectomy (LC) far more frequently than the open procedure. It can result in symptomatic abscess formation, and given its relative rarity, can present a diagnostic challenge. We present the case of a lady whose dropped gallstone resulted in a peritoneo-cutaneous fistula, over 20 years on from her LC.
INTRODUCTION
The benefits of the laparoscopic approach to cholecystectomy are well documented and this is reflected in its adoption as the standard of care for symptomatic gallstone disease [1]. Despite its advantages, its increasing prevalence has resulted in so-called ‘diseases of medical progress’; complications singular to the laparoscopic approach which were not encountered prior to the advent of laparoscopy in the 1980s. A notable example being the spillage of stones from the gallbladder, which can occur as a result of direct trauma during trocar insertion, or mechanically as the gallbladder is manipulated laparoscopically or with compressive force as the specimen is pulled through a port site.
Literature review suggests that even when such a spillage is noted and acted on intra-operatively (with retrieval and washout), retention of a dropped stone within the peritoneal cavity or port site tract can result in a symptomatic abscess in as many as 1% of patients receiving laparoscopic cholecystectomy (LC) [2].
We present the case of a lady whose dropped gallstone resulted in a peritoneo-cutaneous fistula, over 20 years on from her LC.
CASE
A 73-year-old lady presented to her GP with a 3-month history of pain present in the lower back and right buttock on walking. Additionally, she had noted a swelling over the right flank which was intermittently painful. Her background included well controlled hypertension, three normal vaginal deliveries, and an elective LC carried out for biliary colic in a DGH in North West England 20 years previously. She had never smoked, was a trivial drinker, and lived independently.
Her GP examined her and noted an indurated, non-tender lump, 6 cm in diameter, immediately postero-lateral the crest of the right ilium. Weight-bearing and rotational movements of the hip were pain-free, however, extension and flexion at the right hip would reproduce her symptoms. Plain films of the pelvis and both hips demonstrated mild bilateral degenerative change only. A sarcoma of the posterior abdominal wall was suspected and so an urgent outpatient MR scan of the abdomen and pelvis was arranged (Fig. 1).
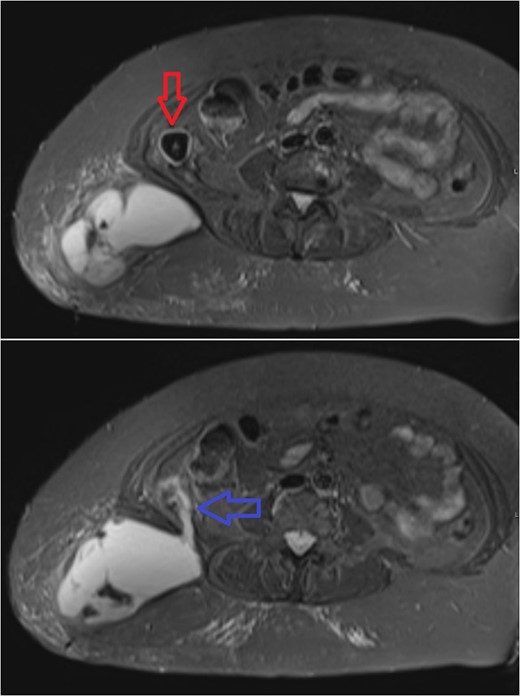
Subsequent axial MR sections of the pelvis. In the first image a large superficial collection can be seen in the soft tissues of the right lower back with surrounding fat stranding. A partially calcified, roughly spherical mass (3 cm in diameter) can be seen, walled-off within the abdominal cavity (red arrow). The second, more inferior section demonstrates communication (blue arrow) between the abscess cavity, through the belly of quadratus lumborum, and the calcified mass.
The study showed an abscess in the superficial tissues of the right lower back, communicating with a partially calcified mass in the right para-colic gutter. The presence of the mass as a likely infectious focus precluded percutaneous drainage and so the patient was referred to a general surgeon. She remained systemically well, and baseline investigations showed a normal white cell count, and only modestly elevated CRP levels at 53 mg dm−3. Abscess formation secondary to a dropped gallstone from her historical procedure was diagnosed, and she was listed for laparoscopic retrieval of the calculus with drainage of the abscess.
By the time of operation, the mass on her right flank had become inflamed, and purulent discharge from a central punctum was noted.
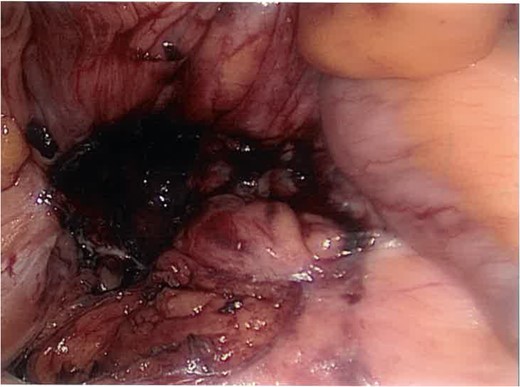
Intra-operatively multiple adhesions were lysed, and the caecum was found to be adherent to the posterior wall. It was freed up and inverted to reveal an inflammatory mass in the right para-colic gutter underlying the ascending colon. Dissection of the overlying inflamed tissue revealed a walled-off gallstone (Fig. 2).

Laparoscopic view of the dropped stone in the right para-colic gutter (caecum inverted top right).
The stone was retrieved (Fig. 4) and the cavity debrided and washed-out. Figure 3 shows the same cavity following excision of the offending stone.
Post-excision laparoscopic view of the posterior abdominal wall cavity.
Upon completion of the laparoscopy the patient was turned to the left lateral position for incision and drainage of the abscess. A peritoneo-cutaneous fistula had indeed formed, ~8 cm in diameter at its mouth. This was drained, washed-out, packed, and left to heal by secondary intention. Swabs from the abscess cavity grew Escherichia coli and Bacteroides species.
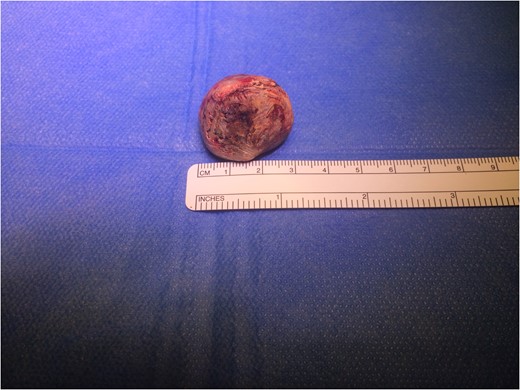
A 3 cm mixed pigment cholelith excised from the abdominal cavity, presumably dropped at laparoscopic cholecystectomy over 20 years previously.
The patient received a short course of oral antibiotic (1 week cefaclor and metronidazole) therapy at discharge. She was followed up as an outpatient 4 weeks later. The sinus had reduced in diameter to ~4 cm and intermittently discharged serous fluid, but the surrounding skin was free of erythema, and there was no clinical evidence of ongoing infection. Her pain on hip flexion/extension was significantly diminished and she was pleased with her outcome. She was discharged to the care of the community nursing team who will continue to pack the sinus until it has closed satisfactorily.
DISCUSSION
This lady’s case is unusual given the length of time between when the stone was (presumably) dropped and the onset of her symptoms (the median onset for such cases being ~5 months [3]). Literature review suggests spillage of gallstones at LC is reported in as many as 40% of procedures [4], however, fewer than 1% of these cases prove symptomatic, and washout at the time of LC is considered a sufficient management technique (i.e. conversion to open is not indicated given our current evidence base) [2]. Calculi that are left behind however, can migrate to a plethora of unusual locations [5, 6], and may present radiologists with diagnostic challenges, particularly when the calculus itself is not radio-opaque, the surrounding inflammatory change may be mistaken for an intra-abdominal neoplastic process [7].
This case adds to the multitude of potential presenting patterns for abscesses secondary to dropped gallstones, and the vanishingly rare incidence of cases of peritoneo-cutaneous fistulae secondary to dropped gallstones (cf cholecysto-cutaneous fistulae seen in active cholecystitis)
The authors speculate that this lady’s pain on walking may be explained by contraction of quadratus lumborum about the abscess as it elevated the ilium during the swing phase of gait, but the delay in abscess formation and presentation remains unaccounted for.
CONFLICT OF INTEREST STATEMENT
None declared.



